Translate this page into:
Drug-induced hemolytic uremic syndrome
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Interferon (IFN) therapy is rarely associated with renal side effects.[1] Among histological findings detected, there are some reports with renal thrombotic microangiopathy (TMA).[2–5] We report here a case of interferon-induced hemolytic uremic syndrome (HUS). A 36-year-old Caucasian woman was admitted for acute renal failure and pulmonary edema. Three years ago, she was diagnosed with multiple sclerosis and received a course of prednisone for 2 months. Later she did not receive any other therapy. Blood pressure and results of renal function tests were always normal. Three months before the admission, because of new radiological findings in brain, the patient was started on IFN-β-1a treatment (22 μg thrice weekly); 7 days before the admission, she began to suffer from asthenia, gain in weight and dyspnea. IFN therapy was withdrawn. Up to admission, the patient received 35 doses of IFN. On admission, physical examination showed high blood pressure and severe pleural effusion without neurological or dermatological findings. We found laboratory features of microangiopathic hemolytic anemia. Immunological (Anti-Neutrophil Cytoplasm Antibodies, Anti-Nuclear Antibodies, Anti-double-stranded DNA antibodies, Anti-Extractable Nuclear Antigen Antibodies, anti-phospholipids-Antibodies) and microbiological laboratory tests were unremarkable. Renal biopsy disclosed signs of thrombotic microangiopathy; among 43 glomeruli, light microscopy revealed focal ischemic signs and mild mesangial cell proliferation; vessel narrowing with thrombi and thickening of arteriolar walls and intimal onion skin-like swelling; light interstitial lymphomonocytic infiltration; and focal tubular atrophy [Figures 1 and 2]. Immunofluorescence showed mesangial IgM, C1q and fibrinogen staining. A diagnosis of HUS was made. She was treated with transfusions, hemodialysis, plasma exchange and methylprednisolone i.v. followed by oral prednisone. Cardiac function improved, and hematological signs progressively disappeared but renal function didn’t recover. IFN-beta treatment was discontinued. Now she is on peritoneal dialysis.
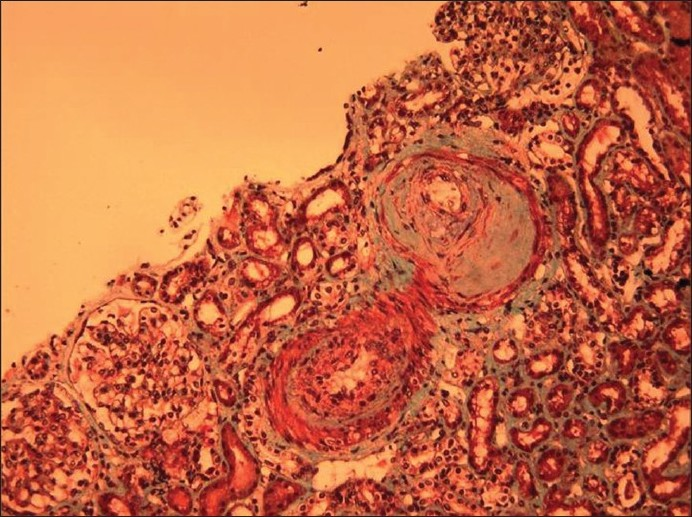
- Intralobular arteries have narrowed lumina due to marked intimal expansion; with edema, mucoid changes, myointimal hyperplasia and sclerosis. The glomerulus shows segmental mesangiolysis with coalescence of some capillary loops. Profiles of dilated tubular lumina contain fragmented erythrocytes. The interstitium appears widened by edema, and there are areas of sclerosis and inflammation (Masson trichrome stain)

- Laminations in the fibrotic intima give the intralobular artery an “onion skin” pattern. The glomerulus on the left has prominent segmental mesangiolysis with formation of capillary microaneurysms. Degenerating red blood cell casts are present in some tubules. There are interstitial fibrosis and mild focal interstitial infiltration of mononuclear leukocytes (Masson trichrome stain)
The mechanism for the development of TMA associated with IFN is not clear. Interferon, such as TNF, IL-1; and free radicals can participate in tissue injury and endothelial cell damage with the resulting deleterious effects. It can exert complex immunomodulatory effects on endothelial cells with differential effects on various endothelial cell surface markers, including the major histocompatibility complex antigens and intracellular adhesion molecules. It can induce modulation of fibrinolytic response of endothelial cells through a prothrombotic way. The release of platelet-aggregating agents from the damaged endothelial cells is probably the final event, resulting in intraluminal thrombus formation and organ damage.
In conclusion, in our patient the temporal association suggests a direct causal effect between IFN therapy and HUS.
References
- Minimal change disease with interferon-beta therapy for relapsing remitting multiple sclerosis. NDT Plus. 2010;3:132-4.
- [Google Scholar]
- Renal thrombotic microangiopathy induced by interferon alpha. Nephrol Dial Transplant. 2001;16:2111-2.
- [Google Scholar]
- Renal thrombotic microangiopathy induced by interferon-alpha. Nephrol Dial Transplant. 2001;16:846-8.
- [Google Scholar]
- Thrombotic microangiopathy in a patient with chronic myelocitic leukemia treated with alpha-interferon. Nephrol Dial Transplant. 1999;14:2469-71.
- [Google Scholar]
- Thrombotic microangiopathy associated with alpha-interferon therapy for chronic myeloid leukemia. Nephrology (Carlton). 2006;11:49-52.
- [Google Scholar]






