Translate this page into:
Polyarteritis nodosa presenting with spontaneous perirenal hematoma
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spontaneous perirenal hematoma following ruptured microaneurysm is an unusual but serious complication of polyarteritis nodosa. We describe a young male who presented with spontaneous perirenal hematoma and was subsequently diagnosed to have polyarteritis nodosa. He was managed with immunosuppressive medications with no recurrence of symptoms.
Keywords
perirenal hematoma
polyarteritis nodosa
vasculitis
Introduction
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis of small and medium-sized muscular arteries. The renal arteries are often involved and intrarenal microaneurysms may be found in 47–60% of cases.[1] Spontaneous perirenal bleeding secondary to PAN was first described by Schmidt[2] in 1908. It occurs in up to 4–13% of cases[3–6] and can be unilateral or bilateral.[7] We reported here a young male who presented with right flank pain and was diagnosed to have spontaneous perinephric hemorrhage secondary to PAN.
Case Report
A 26-years-old student was detected to have hypertension 6 months prior to admission. Since the last 3 months, he complained of mild to moderate intermittent fever along with generalized myalgia and arthralgia of small joints. Over the last 1 month, he developed right flank pain that was dull, persistent, without any aggravating or relieving factor. Though there was moderate weight loss, he denied nausea, vomiting, or black stools and had no history of trauma, bleeding diathesis, or anticoagulant therapy. There was no history of rash, oral ulcers, or photosensitivity. There was also no history of oliguria, hematuria, graveluria, cough, or shortness of breath. Physical examination revealed moderate pallor and a blood pressure of 110/70 mmHg (on two antihypertensive drugs). There were no cutaneous lesions or lymphadenopathy. There was moderate hepatosplenomegaly and a palpable mass in the right para-umbilical region that was firm, mildly tender, nonmobile with vague margins. Other systems were normal and there was no hypertensive retinopathy. Laboratory evaluation revealed hemoglobin 7.2 gm/dL, white blood cell count 10,000 cell/cmm with normal differential count and platelets 3.05 lacs/cmm. Coagulation parameters were normal. Biochemical parameters were urea 51mg/dL, creatinine 1.5 mg/dL, bilirubin 0.8 mg/dL, SGOT/SGPT 36/298 IU, total protein/albumin 7.6/4.3 gm/dL, alkaline phosphatase 71U/L, Ca/P 9.1/3.5 mg/dL. Urinalysis showed microscopic hematuria and 2+ proteinuria and 24 h urine protein was 0.8 gm. Hepatitis B surface antigen, antinuclear antibody (ANA) and antineutrophil cytoplasmic antibodies (ANCA) were negative.
Abdominal ultrasonography and contrast enhanced computed tomography (CT) revealed a right subcapsular renal hematoma with partially thrombosed pseudoaneurysm at the lower pole [Figure 1]. CT scan and CT-angiography also revealed bilateral, multiple aneurysms in kidneys and infarcts in both kidneys and spleen [Figure 2]. A pigtail drainage of the perirenal hematoma was done but did not drain much blood and so was removed. A diagnosis of PAN was made. He was given three doses of intravenous methyl prednisolone (1 gm each) followed by intravenous cyclophosphamide (750 mg/m2). After three pulses of intravenous cyclophosphamide, he was shifted to azathioprine along with low-dose steroids. He remained asymptomatic with no recurrence of symptoms at 6 months of follow up and his blood pressure was controlled on one drug.

- CECT scan showing a large right perinephric hematoma pushing kidney anteriorly with infarction in both kidneys and spleen
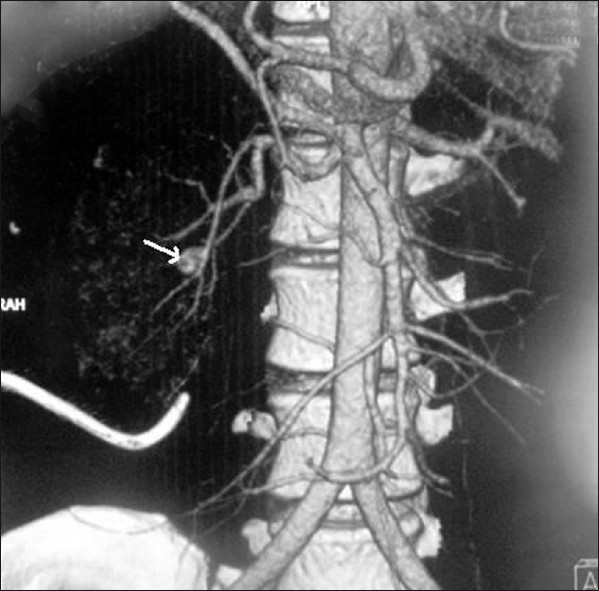
- CT angiogram indicating multiple microaneurysms and one large aneurysm (arrow) in the right kidney with pigtail in situ
Discussion
The 1994 Chapel Hill consensus conference on systemic vasculitides defined classic PAN as “necrotizing inflammation of medium sized or small arteries that spares the smallest blood vessels (arterioles, venules, and capillaries) and is not associated with glomerulonephritis.[8] Most cases of PAN occur in the fourth or fifth decade, although it can occur at any age and there is male preponderance. An association with hepatitis B virus infection is well documented in 7–36% of cases.[9]
It typically develops subacutely with the onset of constitutional symptoms. Livedo reticularis, nodules, mononeuritis multiplex, abdominal pain, and testicular involvement are well-described features. Renal involvement in PAN is in the form of microaneurysms, multiple renal infarcts, proteinuria, hypertension, and renal insufficiency.[10]
Either demonstration of vasculitis on biopsy of involved organs or microaneurysms in involved vessels on angiography are sufficient to make the diagnosis. The American College of Rheumatology criteria (1990) for PAN (3 or more ACR criteria yield 82% sensitivity and 87% specificity for diagnosis) are also useful for diagnosing PAN.[9]
Spontaneous retroperitoneal hemorrhage is a rare life-threatening condition. The etiology includes mostly renal neoplasms such as angiomyolipomas and renal cell carcinomas.[3] Other causes are vascular diseases, infections, cystic diseases, hydronephrosis, preeclampsia, and blood dyscrasias. Among vascular diseases, polyarteritis nodosa is an important cause, others being renal artery dissection, rupture or post renal biopsy.[3] This unusual and serious entity generally results from rupture of an intraparenchymal aneurysm. Factors that may enhance the risk of rupture include severe uncontrolled hypertension, thrombocytopenia, and pregnancy.[11] The common clinical presentation of these patients are acute onset flank or upper abdominal pain, gross hematuria, a palpable abdominal mass or signs of blood loss.[12] In addition to kidneys, spontaneous bleeding may occur in many organs in PAN following rupture of microaneurysm or focal arteritis with consequent infarction. It may present with hemoperitoneum when it involves pancreas,[13] liver[14] or spleen.[15] Massive pulmonary hemorrhage and subarachnoid hemorrhage has also been reported when it involves lung[16] and brain.[17] Sigmoid perforation and mesocolic hematoma has also been reported in a patient with polyarteritis nodosa.[18] Most of the cases of spontaneous bleeding in association with PAN were established antemortem but in few cases diagnosis could be established only post autopsy.[17] Perirenal hemorrhage can be unilateral and bilateral with or without involvement of other organs.[15]
Our patient was diagnosed as PAN in view of fever, weight loss, abdominal pain, hypertension, and multiple, bilateral renal microaneurysms on angiography. Involvement of the splenic arteries is a rare occurrence in polyarteritis nodosa.[15] In our patient there were multiple hypodense lesions in spleen in CT scan. Most probably these were splenic infarcts secondary to involvement of splenic arteries.
A ruptured aneurysm resulting in a huge perirenal hematoma usually necessitates an emergency operation. Sometimes urgent nephrectomy is life-saving.[19] But few cases can be treated by a conservative drainage of the hematoma as in our case or by selective arterial embolization.[20] A concomitant immunosuppressive therapy may be warranted in active disease.
Source of Support: Nil
Conflict of Interest: None declared.
References
- The incidence of microaneurysm in polyarteritis nodosa. Cardiovasc Intervent Radiol. 1986;9:123-6.
- [Google Scholar]
- Etiology of spontaneous perirenal hemorrhage: a meta-analysis. J Urol. 2002;167:1593-6.
- [Google Scholar]
- Spontaneous kidney rupture in polyarteritis nodosa. Report of four cases. Eur Urol. 1988;15:153-5.
- [Google Scholar]
- The evaluation and management of spontaneous perirenal hemorrhage. J Urol. 1980;123:764-5.
- [Google Scholar]
- Perirenal haematoma as the presenting feature of polyarteritis nodosa: is it more common in Turkey? Nephrol Dial Transplant. 1997;12:582-4.
- [Google Scholar]
- Bilateral kidney rupture with severe retroperitoneal bleeding in polyarteritis nodosa. Neth J Med. 1989;35:260-6.
- [Google Scholar]
- Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994;37:187-92.
- [Google Scholar]
- The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990;33:1088-93.
- [Google Scholar]
- Hyperreninemic hypertension secondary to a subcapsular perinephric hematoma in a patient with polyarteritis nodosa. Am J Kidney Dis. 1998;32:503-7.
- [Google Scholar]
- Spontaneous bilateral perirenal hematomas in two patients with eclampsia. J Nephrol. 2003;16:267-71.
- [Google Scholar]
- Spontaneous perirenal hemorrhage: a 10-year experience at our institution. Int Urol Nephrol. 2004;36:15-9.
- [Google Scholar]
- Periarteritis nodosa complicated by intrapancreatic vascular rupture. Gastroenterol Clin Biol. 1988;12:661-3.
- [Google Scholar]
- Polyarteritis nodosa presenting with splenic infarction, bilateral renal infarction, and hematoma. South Med J. 2009;102:972-3.
- [Google Scholar]
- Massive pulmonary hemorrhage in polyarteritis nodosa (PN); report of a case. Jpn J Med. 1990;29:216-21.
- [Google Scholar]
- Polyarteritis nodosa in association with subarachnoid hemorrhage. Intern Med. 2006;45:655-8.
- [Google Scholar]
- Perforation of the sigmoid colon with ischemic change due to polyarteritis nodosa. J Gastroenterol. 1999;34:400-4.
- [Google Scholar]
- Renal hemorrhage in polyarteritis nodosa: diagnosis and management. Am J Kidney Dis. 1999;33:e8.
- [Google Scholar]
- Embolization of two bleeding aneurysms with platinum coils in a patient with polyarteritis nodosa. J Rheumatol. 1993;20:158-61.
- [Google Scholar]







