Translate this page into:
Encephalopathy secondary to isoniazid in patients on hemodialysis
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report isoniazid (INH)-induced encephalopathy in two male patients on hemodialysis. One of them had tuberculous adenitis, and the other had pulmonary tuberculosis. Both were given rifampicin, INH, pyrazinamide, and ethambutol with pyridoxine 40 mg/day. Two patients developed disturbances in consciousness. After excluding other causes, INH-induced encephalopathy was suspected so the drug was stopped and dose of pyridoxine increased. Both patients retained their consciousness within 1 week and were discharged.
Keywords
Encephalopathy
end-stage renal failure
tuberculosis
Introduction
Patients with end-stage renal disease (ESRD) have a high incidence of tuberculosis. Isoniazid (INH) is an anti-tuberculosis drug with well-known neurological side effects including encephalopathy. In this report, we present two cases of INH-induced encephalopathy in patients with ESRD who received anti-tuberculosis therapy for treating tuberculous adenitis and pulmonary tuberculosis.
Case Reports
Case 1
This 48-year-old-male patient was a known case of end-stage renal failure secondary to diabetic nephropathy and was on regular hemodialysis three times per week for the last 10 months. He was diagnosed as having tuberculosis of the mediastinal lymph node by biopsy 5 months before this presentation. He was treated with rifampicin and INH 300 mg/day in addition to pyrazinamide and ethambutol for first 2 months; pyridoxine 40 mg/day was then added to prevent complications. The patient′s consciousness had deteriorated 3 days before presenting to us; no fever, jaundice, vomiting or headache, and no weakness in any part of the body were observed.
On examination, patient was unconscious with Glasgow Coma Scale of 4, temperature was 36.9°C, blood pressure 126/65 and pulse 70/min, and neck stiffness was negative. Pupils were of normal size and shape, all limbs were flaccid with normal-to-depressed reflexes, planters were down, his chest and hearts in addition to abdomen examination were normal. Therefore, as a differential diagnosis, tuberculous meningitis, encephalitis, and metabolic versus ischemic or toxic encephalopathy were suspected.
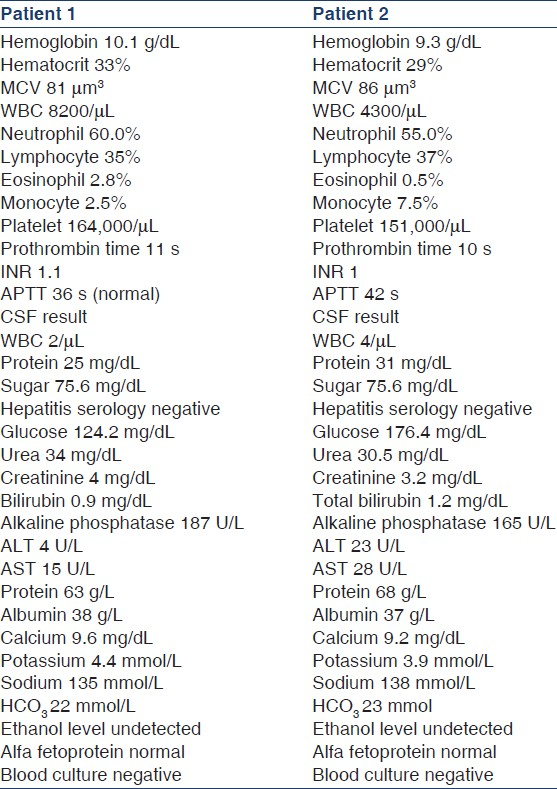
His biochemistry and cerebrospinal fluid analysis [Table 1] was unremarkable apart from his renal failure; computed tomography and magnetic radio-imaging of the brain was normal, electroencephalogram showed diffuse theta slow wave all over the brain. Computed tomography of the abdomen and chest was performed to visualize the lymph node and rule out paraneoplastic, which showed mild thickening of the rectosigmoid junction; further, sigmoidoscopy was performed with biopsy, which was normal. Thus, from this presentation and since there was no evidence of neither organic nor metabolic or infectious cause, an INH-induced encephalopathy was suspected (there is no INH level in our laboratory); therefore, INH was stopped and the dose of pyridoxine was increased. After 2 days, the patient could open his eyes and within 7 days he was completely normal and was discharged, with 400 mg/day moxifloxacine as replacement for INH.
Case 2
This 72-year-old male patient is a known case of end-stage renal failure for the last 2 years secondary to diabetic nephropathy and was on regular hemodialysis three times per week. He was diagnosed as pulmonary tuberculosis 4 months before presentation and started on ethambutol 800 mg every alternate day and pyrazinamide 1200 mg/day for first 2 months, rifampicin 600 mg/day, and INH 300 mg/day with pyridoxine 40 mg/day. He was admitted to the intensive care unit because of deterioration in the level of consciousness 3 days before admission; no other significant history was found.
On examination, the patient was unconscious, could open his eyes to loud voice, with Glasgow Coma Scale of 7, temperature was 37°C; other vital signs were normal, no neck stiffness and other focal neurological sign were recorded, and other system examinations showed unremarkable results. The cerebrospinal fluid analysis was normal; biochemistry test results were normal, apart from renal failure. Also, all septic work up with blood cultures showed negative result. Computed tomography of the brain showed brain atrophy, electroencephalogram showed diffuse slow wave all over the brain. As all septic work up, vascular and organic neurological causes were excluded, an INH toxicity was suspected (there is no INH level in our laboratory); hence, it was stopped and pyridoxine in a dose of 80 mg/day was given through a nasogastric tube. On day 5, the patient was completely conscious and discharged from the intensive care unit on moxifloxacine 400 mg/day as a replacement for INH.
Discussion
The incidence of tuberculosis in patients with ESRD is reported to be 10-fold greater than that of the normal population due to decreased cellular immunity in uremic patients.[1–3] Moreover, increased incidence of side effects secondary to anti-tuberculosis drug treatment in ESRD has been reported.[4]
INH is one of the first line drugs used in the treatment of tuberculosis. It is metabolized in the liver by an acetylation process. The level of INH in the plasma depends on the genetic control; those with autosomal recessive traits show a higher plasma level as they are slow acetylator, whereas those with autosomal dominant traits have a lower level as they are fast acetylator. INH is excreted primarily in the urine in both free and acetylated forms and the dosage of INH may need to be reduced in uremic patients.[5]
The neurotoxic syndrome associated with INH therapy is a well known. Features range from peripheral neuropathy, optic neuritis, encephalopathy, ataxia, dysarthria, and seizure to psychiatric manifestations such as anxiety, depression, paranoid features, schizophreniform psychosis, obsessive compulsive neurosis, and mania.[6] INH induces these effects by inhibiting the phosphorylation of pyridoxine, resulting in a decreased production of pyridoxal-5-phosphate, a co-enzyme involved in multiple metabolic functions, including neurotransmission.[3] Also, acetylation of INH is decreased in ESRD leading to a longer half-life of the drug.[7] There are reported cases with ESRD who developed encephalopathy and cerebellar syndrome while on regular pyridoxine, as observed in our patients.[689] Thus, it would be difficult to determine the adequate dose of pyridoxine to avoid toxicity while not inhibiting the effect of INH.
Conclusion
The reported study in the literature and these two cases suggest that encephalopathy should be taken into consideration when INH is used in ESRD patients undergoing hemodialysis, and the patient should be followed up at regular intervals during the course of anti-tuberculosis therapy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Increased incidence of tuberculosis in patients undergoing hemodialysis. Nephron. 1996;73:421-4.
- [Google Scholar]
- Side-effects of antituberculosis drug treatment in patients with chronic renal failure. Eur Respir J. 2002;20:440-3.
- [Google Scholar]
- Isoniazid-induced neurotoxicity in chronic dialysis patients: Report of three cases and a review of the literature. Nephron. 1993;64:303-6.
- [Google Scholar]
- Isoniazid induced encephalopathy in dialysis patients. Tuber Lung Dis. 1993;74:136-9.
- [Google Scholar]
- Decreased acetylation of isoniazid in chronic renal failure. Clin Pharmacol Ther. 1993;54:612-20.
- [Google Scholar]
- Is isoniazid ototoxic in patients undergoing hemodialysis? Nephron. 2002;92:478-80.
- [Google Scholar]







