Translate this page into:
Transjugular renal biopsy in a case of nephrotic syndrome with extrahepatic portal venous obstruction
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Renal biopsy in patients with nephrotic syndrome helps to establish the pathological diagnosis and subsequent treatment. In certain circumstances, biopsies are difficult to obtain because of the risk of bleeding. We report a case where renal biopsy was obtained through the transjugular route in a patient who had nephrotic syndrome with extrahepatic portal venous obstruction.
Keywords
Nephrotic syndrome
renal biopsy
transjugular
Introduction
Considerable literature exists regarding the presence of renal disease in patients with liver disease. Most of these studies are in patients with hepatitis virus infection, and in established cases of cirrhosis of liver. In majority of these studies, renal pathological evaluation is often limited because of the presence of hypersplenism/bleeding abnormalities. The presence of hypersplenism and its attendant pancytopenia makes biopsies difficult. We report the safe use of the transjugular approach for a simultaneous renal biopsy in a patient with extrahepatic portal venous obstruction and nephrotic syndrome who was offered partial splenic embolization for his portal hypertension.
Case Report
A 25-year-old male patient, a known case of extrahepatic portal venous obstruction and portal hypertension, was detected to have nephrotic syndrome during his pre-anesthetic evaluation for hydrocele surgery. He was told that his surgery was deferred till his kidney disease was evaluated and treated. It was felt that the worsening ascites and subsequent scrotal swelling was aggravated by the presence of his nephrotic state, and hence correction of his nephrotic state will reduce post-operative complications and recurrence of his scrotal swelling. He was subsequently referred to our hospital for his renal evaluation and management.
At the age of 12 years, he had an episode of hematemesis and was evaluated and found to have esophageal varices. Evaluation of his portal hypertension revealed the presence of extrahepatic portal venous obstruction. He was managed with oral propranolol. He stayed asymptomatic except for minimal ascites. His liver functions on regular follow-up stayed normal.
Three months prior to this admission, he started developing scrotal swelling, abdominal distension and pedal edema for which he consulted a surgeon. Physical examination revealed pallor, pedal oedema, tense ascites, splenomegaly and bilateral hydrocele. Laboratory investigations showed evidence of anemia, thrombocytopenia, renal insufficiency hypoalbuminemia, and normal liver enzymes. His coagulation work up was normal. His cardiac evaluation did not reveal any abnormality. His urine analysis revealed the presence of proteinuria. Ultrasonography of the abdomen showed massive splenomegaly, ascites and no evidence of liver cirrhosis. Liver biopsy showed normal liver architecture with no abnormality. Adiagnosis of nephrotic syndrome was made and the bilateral hydrocele repair was postponed, and the patient was referred to the Nephrology services of our hospital for the management of nephrotic syndrome and renal insufficiency.
The laboratory investigations in our hospital are shown in Table 1.

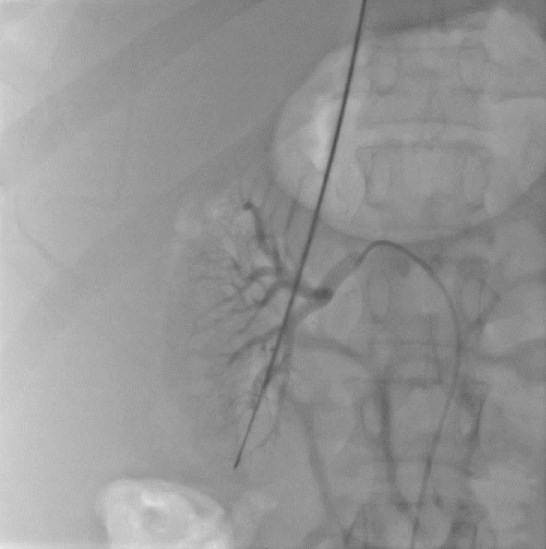
A renal biopsy was advised for histopathological diagnosis. However, due to pancytopenia and tense ascitis, a percutaneous renal biopsy was deferred and open renal biopsy was considered. An open surgical biopsy was also considered risky as the anatomical position of his kidneys necessitated 12th rib resection for renal access. The case was discussed with the interventional radiologists whose opinion was sought for management of hypersplenism. It was felt that during his partial splenic embolisation via the transjugular route, a renal biopsy can be performed. Transjugular renal biopsy along with splenic embolization was thus advised and after optimisation with blood and blood products the patient underwent both the procedures in the same sitting. For the transjugular renal biopsy, 8 Fr guiding sheath was guided into the lower pole of right (R) renal vein. The long transjugular liver biopsy needle (Cook USA) was used to get a core biopsy. The needle tip was protected with a 5 Fr catheter. Under fluoroscopic control, the needle was positioned deep in the vein, allowing the tip to protrude into the renal cortex [Figure 1]. No post procedure complications like drop in hematocrit, gross hematuria or perirenal hematoma were encountered.
- Transjugular renal biopsy
Post procedure his platelet counts improved to 120,000/μL (vs. 77,000) and WBC count to 16,300, three days after the splenic embolization. However, the biopsy specimen was inadequate for an opinion and a re-biopsy through the transjugular approach was done with no complications [Figure 1]. Biopsy was suggestive of minimal change disease. He was started on oral steroids. His condition gradually improved with resolution of pallor and pedal edema and ascites. Pre-steroid urine protein/creatinine ratio was 11.67 which improved to 3.02 after 1week of steroids and ACE inhibitors. His haemoglobin and albumin levels improved subsequently. He underwent bilateral hydocele repair successfully with no complications. Predischarge he received his pneumococcal vaccination. He is now asymptomatic and under regular follow-up. At 6-months post follow-up, he was in clinical and biochemical remission for his nephrotic syndrome and had normal renal functions.
Discussion
Renal glomerular changes are well recognized in patients with liver disease. Membranous and membranoproliferative glomerulonephritis have been described with hepatitis B and Hepatitis C infection.[12] There are case reports of association of minimal change nephropathy with chronic hepatitis C infection.[3] However, glomerular lesions are not as common as ATN/AKI in cirrhosis of liver.[4] In patients with non-cirrhotic portal hypertension, IgA nephropathy appears to be common.[5] Interestingly, there is an increase in incidence of glomerulonephritis in patients with non-cirhhotic portal hypertension who have undergone splenorenal shunt surgery.[6] This study had reported minimal change nephropathy as an uncommon renal lesion (incidence of 3%). Our patient had minimal change nephrotic syndrome on biopsy.
Most patients with liver disease don't undergo indicated renal histological evaluation because of the presence of bleeding abnormalities. In such situations, transjugular renal biopsy may be attempted if the expertise is available. The first report of transjugular renal biopsy appeared in literature 20years back.[7] This procedure is practiced commonly in continental Europe and its experience is limited in USA. However, literature from across the Atlantic consider it safe and effective in high-risk patients.[8–10] The effectiveness of the procedure in the hands of interventional nephrologists is also reported.[11] In certain centers, this procedure is attempted with simultaneous insertion of internal jugular hemodialysis catheter in patients with acute renal failure (ARF).[12] This early availability of renal histology altered the management in 50% of the patients with ARF. The procedure is considered relatively safe with minor complications like renal hematoma, macroscopic hematuria and capsular perforation reported in literature.[81314] Contrast nephrotoxicity has also been reported. Major complications of arterio-pelvicalyceal fistula and renal vein thrombosis are rare.[15] Overall, complication rates are similar to that of percutaneous biopsy. Our patient had no bleeding complications.
The diagnosis of minimal change disease and the consequent treatment with steroids allowed his surgeons to perform the required surgery after 3 months. Six months later he was back to his desk job with no major medical problems.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Associations of various histological morphologies of renal involvement in hepatitis B infection: Analysis of 118 subjects. Saudi J Kidney Dis Transpl. 2010;21:964-6.
- [Google Scholar]
- Hepatitis C virus and kidney: Astrong association with different clinical aspects. Liver Int. 2011;31:1071-80.
- [Google Scholar]
- Minimal-change nephropathy and chronic hepatitis C infection: coincidental or associated? Nephrol Dial Transplant. 2007;22:1479-80.
- [Google Scholar]
- Clinical spectrum of renal disorders in patients with cirrhosis of liver. Ren Fail. 2011;33:40-6.
- [Google Scholar]
- Increased incidence of glomerulonephritis following spleno-renal shunt surgery in non-cirrhotic portal fibrosis. Kidney Int. 1997;52:482-5.
- [Google Scholar]
- Transjugular renal biopsy. Our experience with 67 cases. Kidney Blood Press Res. 2001;24:207-12.
- [Google Scholar]
- Renal biopsy practice in France: Results of a nationwide study. Nephrol Dial Transpolant. 2010;25:3579-85.
- [Google Scholar]
- Transjugular renal biopsy in patients with liver disease. AmJ Kidney Dis. 2001;37:1144-51.
- [Google Scholar]
- Safety and efficacy of transjugular renal biopsy performed by interventional nephrologists. Semin Dial. 2011;24:343-8.
- [Google Scholar]
- Simultaneous transjugular renal biopsy and hemodialysis catheter placement in patients with ARF. Am J Kidney Dis. 2004;44:429-36.
- [Google Scholar]
- Safety and diagnostic yield of transjugular renal biopsy. J Vasc Interv Radiol. 2008;19:546-51.
- [Google Scholar]
- Transjugular kidney biopsy: Enabling safe tissue diagnosis in high risk patients. Isr Med Assoc J. 2011;3:425-7.
- [Google Scholar]







