Translate this page into:
Granulomatous interstitial nephritis: Our experience of 14 patients
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Granulomatous interstitial nephritis (GIN) is a rare condition. Drugs, infections, immune processes, and foreign body reaction are the main causes. We identified a total of 14 patients with GIN during a period of 13 years in 2798 renal biopsies. There were 8 males and 6 females in the age range of 20-70 (mean 35 ± 12) years. The serum creatinine at presentation was 6.7 ± 3.8 (range: 2.3-14.7) mg/dl. In nine patients tuberculosis was the causative agent. Drugs (n = 2) and Wegener's granulomatosis (n = 1) were other etiologies. Systemic lupus erythematosis (SLE) and Immunoglobulin A nephropathy (IgAN) were seen in one patient each. Patients with tuberculosis were treated with antituberculous therapy and three of them improved. Four out of six patients who required dialysis at presentation remained dialysis dependent, one of whom underwent renal transplantation. Two patients progressed to end stage renal disease after 7 years and 9 years each. The patients with drug induced GIN had improvement in renal function after prednisolone treatment. Patients with SLE, and Wegener's granulomatosis responded to immunosuppression. Patient with IgAN was on conservative management. Finally, six patients were on conservative management for chronic renal failure.
Keywords
Drug induced
granulomatous interstitial nephritis
tuberculosis
Introduction
Although acute interstitial nephritis is a common cause of acute kidney injury, granulomatous interstitial nephritis (GIN) remains a rare condition. In the report of Mignon et al.,[1] granulomata were detected in only 0.95% of 3500 patients with renal biopsies. Drugs (37.5%) were the most common agent. Besides drugs, other etiologies commonly associated with GIN include, infections, immune processes, foreign body reaction, and some instances classified as idiopathic. There are not many published studies[123456] of GIN, and none from the Indian subcontinent. Tuberculosis being endemic in India, the causative agents of GIN is likely to be different from the other studies. The aim of the study was to analyze the etiology, clinical features and outcome of patients with biopsy-proven GIN at our institute from January 2000 to October 2012.
Materials and Methods
All renal biopsy records from January 2000 to October 2012 were scrutinized for the diagnosis of GIN. The clinical data were recorded from the case sheets of patients and also from outpatient (OP) records of the discharged patients. OP records were used to know the outcome of patients. The proforma included, the presenting history, past history, drug history, vital data, clinical examination, investigations, and management.
The renal biopsy slides were retrieved and reviewed. All slides were stained with H and E, periodic acid-Schiff, Masson Trichrome, Silver and Ziehl-Neelsen stains. In all patients, deeper sections were taken to expose the entire granuloma. Aggregates of epithelioid histiocytes with or without giant cells within the interstitium or perivascular region were labeled as a granuloma. In addition, the nature of granuloma was assessed for the presence of necrosis, confluence with or without giant cells and Schumann or asteroid bodies.
Patients with tuberculosis were treated with combinations of isoniazid (5 mg/kg/d), rifampin (10 mg/kg/d), pyrazinamide (10 mg/kg/d), ethambutol (5 mg/kg/d) and levofolaxacin (15 mg/kg/q 48 h, post hemodialysis). For the first 3 months four drugs were prescribed and for the next 6 months two drug were continued. No post-treatment prophylaxis was given.
Patients with other causes were treated after work-up for infection. Immunosuppresion was given accordingly with steriods, cyclophosphamide, and azathioprine. The offending factor was withdrawn.
Results
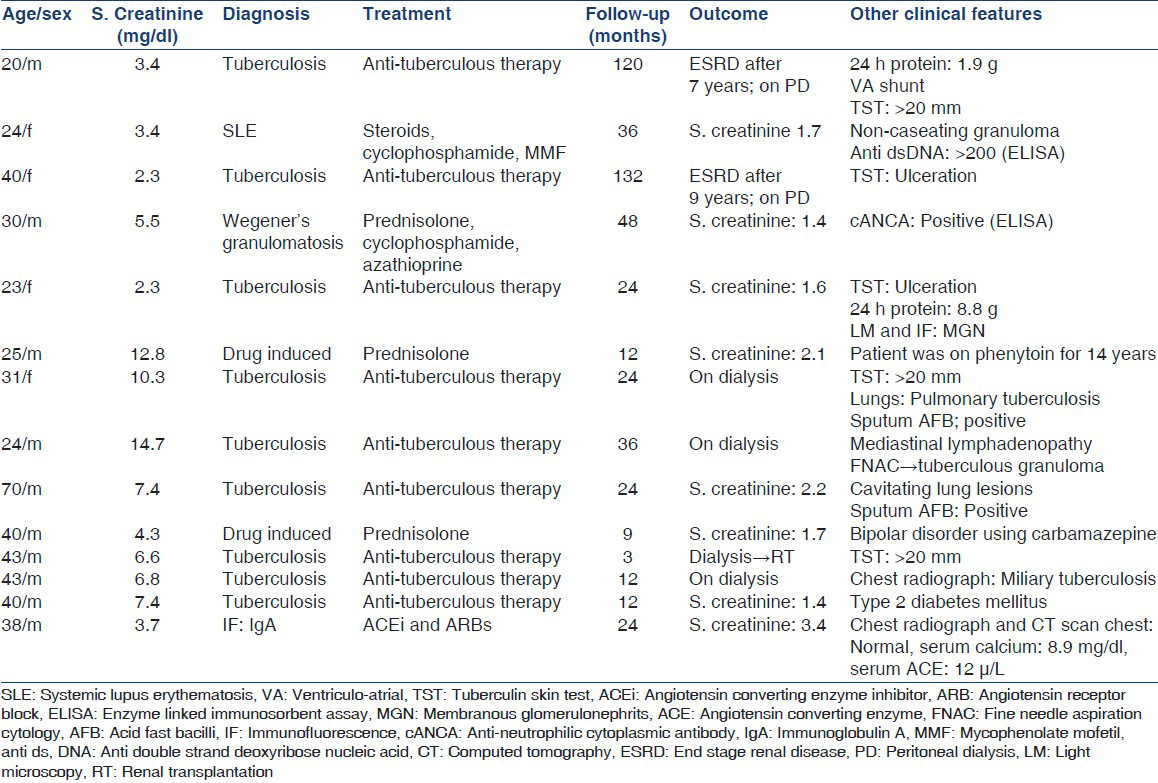
During the 13 year period 2798 renal biopsies were performed at our institute. There were 14 patients with GIN. GIN; therefore, accounted for 0.5% of patients. There were 8 (57.1%) males. The age was 35 ± 12 years, with a range of 20-70 years. All patients presented with renal failure and normal kidney size. The presenting serum creatinine was 6.7 ± 3.8 (range: 2.3-14.7) mg/dl. In nine patients tuberculosis was the causative agent. Drugs (phenytoin and carbamazepine) were the cause in two patients. Wegener's granulomatosis, systemic lupus erythematosis (SLE), and Immunoglobulin A nephropathy (IgAN), were the associated conditions in one patient each. Patient data have been described in Table 1.
Pathology
The number of glomeruli were 11.5 ± 2.5. The number of patients was too small for statistical analysis of pathologic features between etiologic groups. Necrosis was seen in two patients and asteroid bodies in one. Giant cells were present in all the patients, but with varying severity: Scanty (patient numbers: 3, 5, 7, 8, 10, 14) to moderate (patient numbers: 4, 6, 11) to plentiful (patient numbers: 1,2,9,12,13). Tubular atrophy and interstitial fibrosis were present in 8 (57.14%) patients.
Patients with tuberculosis
Pulmonary tuberculosis was demonstrated in patient numbers 7, 9, and 12. Sputum acid-fast bacilli (AFB) were positive in two of them and chest radiograph revealed miliary pattern in one. Mediastinal lymphadenopathy was found on computed tomography scan in one patient number 8. The biopsy of the lymph node revealed caseating granuloma with AFB on Ziehl Neelsen staining. In these four patients, the diagnosis of tuberculosis was made after renal biopsy revealed GIN. In patients numbers 3 and 5 tuberculin skin test (TST) was ulcerated and in patient numbers 1 and 11, TST was >20 mm, suggesting tuberculosis. These seven patients had fever, cough and sputum and anorexia and weight loss.
The serum calcium of all the patients was 8.8 ± 1.2 (range: 7.6-9.5) mg/dl. Hypercalcemia was not found in any patient. Serum angiotensin enzyme concentration was done in one patient only.
Patients with tuberculous GIN were treated with anti-tuberculous therapy. The four patients (patient numbers: 7, 8, 11, and 12) who required dialysis at presentation continued on dialysis. Subsequently one of them underwent renal transplantation. Patient numbers 1 and 3 required dialysis after seven and 9 years each respectively. Patient numbers 5 and 13 had improvement in renal insufficiency after antituberculous therapy. Both patients with drug induced GIN had renal function improvement after prednisolone treatment. SLE patient (patient number 2) and Wegener's granulomatosis (patient number 4) had responded to immunosuppression. Finally, six patients were on conservative management for chronic renal failure.
Discussion
We are herewith reporting 14 patients of GIN. This is the first case series from India. Prior to this there were a few case reports from India.[78910] There were five publications of case series of GIN. Recently, there was a review of GIN in allografts.[11] The age of patients was lower in our patients than these studies. While in our patients tuberculosis was a significant cause of GIN, in the previous studies dugs and sarcoidosis were leading causes and a higher percentage of (42.8%, 6 out of 14) required renal replacement therapy (RRT) in our patients [Table 2].

The mean age was less than the other studies. This could be due to the dominance of tuberculosis. Tuberculosis is common in Indians in the age range of 15-54 years.[12] Mignon et al. and Javaud et al.,[13] reported tuberculosis as a cause of GIN in their series. This study highlights tuberculosis as a cause of GIN. Tuberculosis could also affect kidney by causing amyloidosis and focal proliferative glomerulonephritis.[14] We also reviewed glomerular lesions of tuberculosis.[15] Sarcoidosis and tubulointerstitial nephritis with uveitis (TINU) were not found to be a causative factor in our series. All patients were investigated fully for all possible causes of GIN, once granulomata were found in renal biopsy. Hence, missing the diagnosis of sarcoidosis and TINU was unlikely. Indeed, there were no previous articles published from India reporting GIN with sarcoidosis. Another feature of this article was only one patient had no etiological/diagnosis. The immunofluorescence of this patient suggested IgAN. Despite thorough investigation the cause could not be identified. IgAN presenting as GIN was reported before, but except for one report all had a cause for IgAN.[16] All patients in the present study had raised serum creatinine at presentation. This could explain greater requirement of RRT in our patients. GIN could be isolated or associated with the organ involvement orienting the diagnosis of underlying diagnosis. In the present study in seven patients tuberculosis was identified after GIN was diagnosed on renal biopsy.
In summary, GIN is a rare cause of renal failure with multiple etiology, which are treatable. In Indian subcontinent, tuberculosis is the most common etiology of GIN. Histologic features do not seem to identify the underlying cause of GIN. Clinical manifestations are also varied and do not distinguish the cause of GIN. Treatment of the underlying cause can reverse renal failure if it is not severe enough. In our study, many (42.8%) had stage five chronic kidney diseases.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Isolated sarcoid granulomatous interstitial nephritis: Review of five cases at one center. Clin Nephrol. 2001;55:297-302.
- [Google Scholar]
- Seven cases of granulomatous interstitial nephritis in the absence of extrarenal sarcoid. Nephrol Dial Transplant. 2003;18:280-4.
- [Google Scholar]
- Renal involvement in sarcoidosis: A report of 6 cases. Clin Nephrol. 2002;57:142-8.
- [Google Scholar]
- Renal granulomatous sarcoidosis: Report of six cases. Nephrol Dial Transplant. 1990;5:18-24.
- [Google Scholar]
- Granulomatous interstitial nephritis due to tuberculosis-a rare presentation. Saudi J Kidney Dis Transpl. 2009;20:842-5.
- [Google Scholar]
- Rapidly progressive renal failure a rare presentation of granulomatous interstitial nephritis due to tuberculosis case report and review of literature. NDT Plus. 2011;4:383-5.
- [Google Scholar]
- Idiopathic necrotising granulomatous interstitial nephritis. J Postgrad Med. 2001;47:111-2.
- [Google Scholar]
- Cryptococcal granulomatous interstitial nephritis and dissemination in a patient with untreated lupus nephritis. Nephrol Dial Transplant. 2009;24:3243-5.
- [Google Scholar]
- Granulomatous tubulointerstitial nephritis in a renal allograft: Three cases report and review of literature. Clin Transplant. 2012;26:70-5.
- [Google Scholar]
- Epidemiology of communicable diseases. In: Park K, ed. Park's Textbook of Preventive and Social Medicine (20th ed). Jabalpur (India): M/s Banarsi Das Bhanot; 2009. p. :161.
- [Google Scholar]
- Renal granulomatoses: A retrospective study of 40 cases and review of the literature. Medicine (Baltimore). 2007;86:170-80.
- [Google Scholar]
- Membranous nephropathy and granulomatous interstitial nephritis due to tuberculosis. Clin Nephrol. 2011;76:487-91.
- [Google Scholar]
- Granulomatous interstitial nephritis: A clinicopathologic study of 46 cases from a single institution. Int J Surg Pathol. 2006;14:57-63.
- [Google Scholar]







