Translate this page into:
Valacyclovir associated neurotoxicity in a patient on dialysis
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 58-year-old female patient was admitted with complaints of altered sensorium, irritability and drowsiness since two days. It began when she started feeling drowsy, restless and talking irrelevantly. Confusion and drowsiness worsened further on day two. Patient was diagnosed to have herpetic skin lesions on her right abdomen four days back and started with valacyclovir 500 mg once a day. Patient was a known case of chronic kidney disease (CKD) on maintenance dialysis, hypertensive since 12 years, on medications. On admission, she was afebrile, pulse was 120 bpm, high blood pressure of 210/110 mmHg was recorded, with signs of pallor. Systemic examination was unremarkable. Patient was admitted in intensive care unit. She was monitored and managed for hypertension. Valacyclovir was stopped on day 2. Magnetic resonance imaging (MRI) brain revealed a normal study with no acute changes. Electroencephalography (EEG) showed generalized slowing of brain wave activity, no epileptic discharges. Cerebrospinal fluid (CSF) study was essentially normal. For initial 3 days patient remained to be in a drowsy, disoriented state. She underwent dialysis on day 2 for both markedly deranged kidney function tests and neurotoxicity. After her 2nd dialysis, there was some recovery in her consciousness, which improved with subsequent planned dialysis and she regained normal sensorium by day five. Valacyclovir is a prodrug. It acts by inhibiting viral deoxyribonucleic acid polymerase.
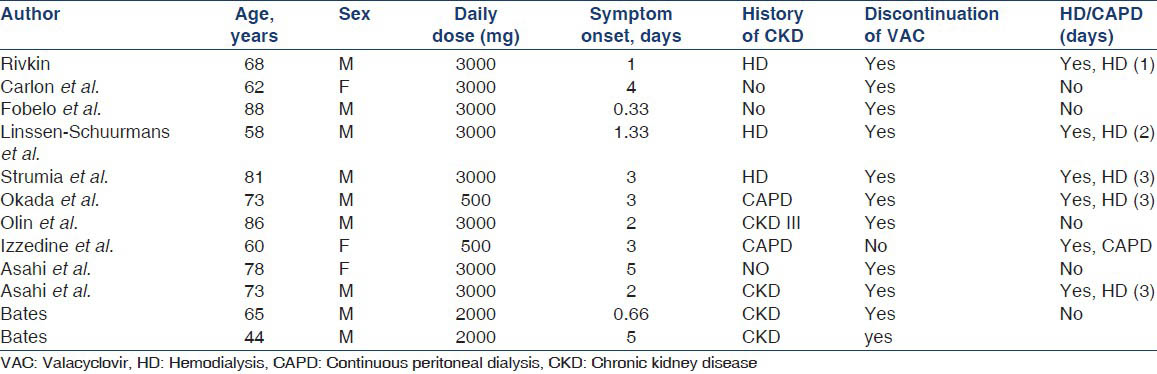
Its use has been introduced recently over acyclovir due to the decrease in frequency of dosing and superior bioavailability. Although neuropsychiatric manifestations with valacyclovir are less frequent, they can commonly manifest as confusion, dizziness, irritability, ataxia, tremors, seizures, myoclonus and hallucinations.[1] Symptoms can occur within 2-3 days of initiation of therapy and resolve within 5-7 days after stopping the dug or hemodialysis is another modality as the drug can be filtered.[1] The results of CSF analysis and computed tomography/MRI brain are usually unremarkable. Plasma levels of the drug do not correlate with its adverse effects. EEG finding commonly encountered is diffuse generalized slowing of brain activity.[2] In several studies reported in past [Table 1][3] it has been shown that occurrence of valacyclovir associated neurotoxicity (VAN) has been common in elderlies, with a daily dose ranging from 500 to 3000 mg/ day, more frequent in CKD patients, treated successfully after discontinuation of drug and requiring at least a single hemodialysis. In our case, a middle aged lady with end stage renal disease on dialysis was prescribed renal dose of valacyclovir, i.e. 500 mg OD. Despite this dose adjustment, she developed neurotoxic side-effects of the drug requiring hospitalization, discontinuation of drug and dialysis, following which symptoms of drug improved and sensorium got better. Valacyclovir can pose a diagnostic dilemma for the clinician as herpes zoster encephalitis and VAN share disturbance in sensorium as most frequent manifestation. Physicians should be aware of neurotoxic potential of valacyclovir and importance of dose adjustment in patient with renal dysfunction. Prompt discontinuation of drug and dialysis can help in improving the outcome.
References
- Valacyclovir neurotoxicity: Two case reports and a review of the literature. Can J Hosp Pharm. 2002;55:123-7.
- [Google Scholar]
- Possible valacyclovir-related neurotoxicity and aseptic meningitis. Ann Pharmacother. 2003;37:1814-7.
- [Google Scholar]
- Neurotoxicity associated with standard doses of valacyclovir in renal insufficiency. Hosp Pharm. 2011;46:774-8.
- [Google Scholar]






