Translate this page into:
Clinical spectrum and outcomes of crescentic glomerulonephritis: A single center experience
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
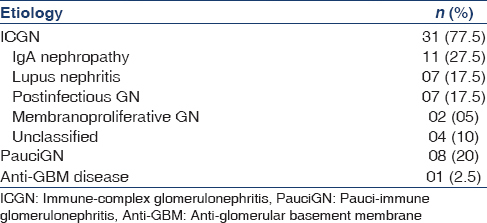
There is limited data on the etiology, clinical and histopathological spectrum and outcomes of crescentic glomerulonephritis (CrGN) in adult Indian population. This prospective study was done to evaluate the etiology, clinicohistological patterns and predictors of outcome of CrGN in South Indian population. All the patients received standard protocol based immunosuppression in addition to supportive care. Immune-complex glomerulonephritis (ICGN) was the most common etiology (n = 31; 77.5%) followed by pauci-immune glomerulonephritis (PauciGN; n = 8; 20%) and anti-glomerular basement membrane disease (n = 1; 2.5%). The most common etiology of ICGN was IgA nephropathy (n = 11; 27.5%) followed by lupus nephritis (n = 7; 17.5%) and post-infectious glomerulonephritis (PIGN) (n = 7; 17.5%). The patients with PauciGN were significantly older compared to those with ICGN (44.5 ± 15 years vs. 31.8 ± 11 years; P = 0.01). The patients with PauciGN presented with significantly higher serum creatinine (9.7 ± 4.4 vs. 6.6 ± 3.3 mg/dl; P = 0.03). The histopathologic parameters of ICGN and PauciGN were comparable except for a higher proportion of sclerosed glomeruli in ICGN. At the end of 3 months follow-up, only two patients went into complete remission (5.4%). Majority of the patients had end-stage renal failure (48.6%) and were dialysis dependent and seven patients (18.9%) expired. There was no signifi difference in the renal survival (10.9 ± 1.9 vs. 9.6 ± 3.3 months) or patient survival (17.5 ± 2.1 vs. 17.3 ± 4.3 months). The parameters associated with adverse outcomes at 3 months were hypertension (odds ratio [OR]: 0.58; confidence interval [CI]: 0.36–0.94), need for renal replacement therapy (OR: 0.19; CI: 0.04–0.9), serum creatinine at admission (P = 0.019), estimated glomerular filtration rate (P = 0.022) and percentage of fibrocellular crescents (P = 0.022).
Keywords
Crescentic glomerulonephritis
immune-complex glomerulonephritis
pauci-immume glomerulonephritis
Introduction
Crescentic glomerulonephritis (CrGN) is a disease with grave prognosis. Retrospective biopsy based series has reported a prevalence varying from 2.1% to 4.2%.[12] There is significant heterogeneity in the etiology and outcomes of CrGN[34] with limited data from India.[5678] There is no published literature on CrGN from south India. This study aims to identify the etiology, assess and compare the clinical features, histomorphological parameters and outcomes of patients with CrGN in South India.
Materials and Methods
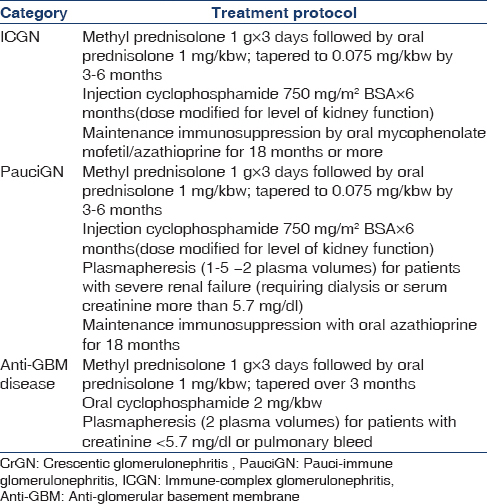
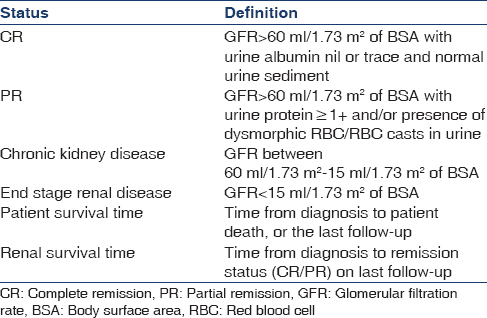
The study population included all adult patients admitted with CrGN from January 2011 to April 2014. Renal biopsy was considered adequate if a minimum number of five glomeruli were present, with >50% crescents. Biopsy specimens were subjected to light (LM) and immunofluorescence microscopy (IF) and reviewed by two independent pathologists blind to the clinical data. All patients were treated according to standard treatment protocols [Table 1]. Patients were followed up with monthly serum creatinine, urine protein, urine microscopy and blood counts. Primary outcomes were analyzed at the end of 3 months [Table 2].
The baseline clinical, biochemical and histopathological parameters and primary outcomes were compared between immune-complex glomerulonephritis (ICGN) and pauci-immune glomerulonephritis (PauciGN). All categorical and ordinal variables were expressed as frequencies and percentages and compared by Chi-square test or Fisher's exact test. Continuous variables were expressed as mean with standard deviation or median with range and compared by independent Student's t-test or Mann–Whitney U-test. Relative risk (RR) along with confidence intervals (CIs) was estimated to assess the risk for the primary outcome. Survival times were compared by log-rank test. A logistic regression analysis was done to assess the predictors of adverse outcomes (death + end-stage renal disease [ESRD]) at 3 months. All the statistical analyses were carried out at 5% level of significance, and P < 0.05 was considered as statistically significant. Data were analyzed using SPSS version 19.0 (IBM Corporation, US).
Results
A total of 728 kidney biopsies were performed during the study period of which 42 had CrGN (5.8%). Two patients were excluded as biopsy was inadequate. Follow-up data were available for 37 patients; duration of follow –up varied from 3 to 27 months. About 92.5% patients had more than 3 months and 45% had more than 1-year follow-up. The etiology of CrGN is given in Table 3. The patients with PauciGN were older compared to ICGN (44.5 ± 15 vs. 31.8 ± 11 years; P = 0.01). There was no difference in the sex ratio between two categories. The clinical, biochemical and histological parameters of the two groups are given in Tables 4–6.
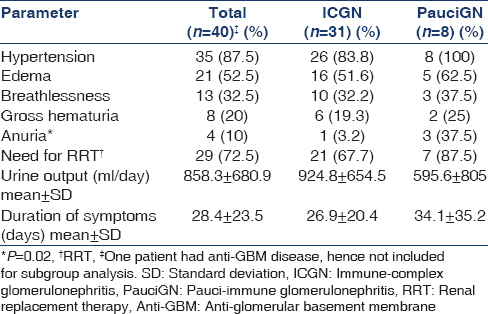
All PauciGN patients had renal limited disease; 5/8 showed positivity for p-ANCA. Plasmapheresis (PP) was given to 7/8 patients with PauciGN and one patient with anti-glomerular basement membrane (GBM) disease.
Treatment and outcomes
The primary outcomes are shown in Table 7. The RR of patients with ICGN for progression to ESRD as well as death was lower when compared to PauciGN (0.74 [0.38–1.5] and 0.38 [0.11–1.36] respectively). The mean patient survival time for ICGN and PauciGN were 17.5 ± 2.1 and 17.3 ± 4.3 months respectively. The mean renal survival time for ICGN was 10.9 ± 1.9 months and PauciGN was 9.6 ± 3.3 months. There was no difference in patient or renal survival (P > 0.05).
The presence of hypertension (odds ratio [OR]: 0.58; CI: 0.36–0.94), need for renal replacement therapy (OR: 0.19; CI: 0.04–0.9), serum creatinine at admission (8.4 ± 3.6 mg/dl vs. 5.4 ± 3.14 mg/dl; P = 0.019), estimated glomerular filtration rate (eGFR) at admission (16.58 ± 13.5 ml/1.73 m2 vs. 8.8 ± 6.4 ml/1.73 m2; P = 0.022) and percentage of fibrocellular crescents (21.9% [±16.5] vs. 11% [±11]; P = 0.022) were associated with adverse outcomes at 3 months.
Discussion
In contrast to existing literature, we observed that ICGN (77.5%) was the most common cause of CrGN. ICGN is the predominant cause of CrGN in the pediatric population, whereas PauciGN is common among adults.[36] The most common etiology of ICGN in the current study was IgA nephropathy followed by lupus and PIGN. A few studies from Asia have reported ICGN as the predominant etiology in adults.[45910] This observation is not surprising considering the high prevalence of IgA nephropathy in Asian countries.[91112] Another interesting observation is the higher proportion of patients with PIGN, a disease that is considered to be common in the pediatric population.[7] The high prevalence of PIGN in the current study might be due to the tropical location and poor socioeconomic conditions predisposing to infections. Even though the age distribution of patients was similar to previous studies, comparison with the existing series might have limitations in view of the different etiologic spectrum.[456]
The histological parameters were comparable in the two groups except for the higher proportion of sclerosed glomeruli in ICGN. This might be secondary to the high proportion of patients with IgA nephropathy and lupus nephritis, which follows a more indolent course[91013] Two-third of PauciGN patients showed ANCA positivity, similar to what reported from previous series.[31415] Renal limited vasculitis as the sole etiology of PauciGN in this series might be secondary to the local reference patterns. Interestingly, two patients with lupus nephritis had p-ANCA positivity, which is considered as an epiphenomenon.[7161718]
In the current study, in spite of early biopsy, absence of significant chronicity and early institution of specific therapy, the prognosis remained poor. The renal survival of CrGN is dependent on the age, etiology, extent of the renal failure and the histological subtype.[3467192021222324] Indian studies on CrGN had reported ESRD rates varying from 14.7% to 52.4%, but in contrast to the current study they had a much lower serum creatinine levels and included pediatric patients, who are known to have better outcomes.[5678] Crescentic IgA and lupus are associated with a poor response, with more than 50% progressing to ESRD.[13212223] Renal function loss is almost universal with serum creatinine levels more than 6 mg/dl.[192223] The probable reasons for higher rate of progression to CKD and ESRD might be secondary to higher mean creatinine concentration as well as a high proportion of IgA nephropathy and lupus which are well-known to be associated with inferior survival. Our mortality rates were higher when compared to another series of adult CrGN from India.[5] The majority of the deaths were due to complications of kidney failure; which occurred after discharge from the hospital, reflecting the suboptimal dialysis facilities available at community level in this part of the country.
In the current study, PauciGN carried a high risk for adverse events in the initial months, but the long-term patient and renal survival were comparable. This dissociation probably results from lesser numbers of PauciGN as well as the presence of renal limited disease that is known to have a less indolent course when compared to another vasculitis.
Similar to previous studies, we found that hypertension, need for renal replacement therapy, serum creatinine, eGFR and percentage of fibrocellular crescents were predictive of adverse outcomes.[37192324] We did not find any association with arteriolar fibroid necrosis, proportion of cellular crescents and tubulointerstitial inflammation as described in other studies.[624]
The merits of our study are a good number of patients with complete clinical, histopathological, and serological and biochemical correlations with good follow-up. All the patients included in the study received uniform protocol based management according to the etiology. The results of the study should be interpreted with the following inherent limitations. This is a single center study with a small sample size, with ICGN outnumbering PauciGN. We could not study the outcomes of anti GBM disease, as only a single case was included in the series. The huge differences in numbers of ICGN and PauciGN could affect the interpretation of subgroup analysis, resulting in a type II error. We did not try to analyze the effect of PP on outcomes, as it was limited to a subgroup of patients as per our treatment protocol. The higher mortality rates on follow-up are secondary to complications of renal failure resulting from suboptimal dialysis facilities at community level rather than the primary disease. Electron microscopy was not part of study protocol due to its nonavailability in our institution. Hence, we couldn't sub-classify four patients with ICGN based on LM and IF alone.
Conclusions
Immune-complex glomerulonephritis is the most common cause of CrGN in this part of the country with IgA nephropathy being the predominant disease. The clinical presentation is marked by severe renal failure at presentation and comparatively lesser response rates, higher mortality and progression to ESRD in spite of strict adherence to standard immunosuppressive therapy. Further research is needed to formulate more aggressive treatment policies to ensure renal as well as patient survival in long-term.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Pattern of glomerular diseases among adults in Rajshahi, the Northern Region of Bangladesh. Saudi J Kidney Dis Transpl. 2012;23:876-80.
- [Google Scholar]
- Glomerulonephritis with crescents among adult Saudi patients outcome and its predictors. Clin Exp Med. 2012;12:121-5.
- [Google Scholar]
- Clinicopathologic spectrum of crescentic glomerulonephritis: A hospital-based study. Saudi J Kidney Dis Transpl. 2014;25:689-96.
- [Google Scholar]
- Crescentic glomerulonephritis: A clinical and histomorphological analysis of 46 cases. Indian J Pathol Microbiol. 2011;54:497-500.
- [Google Scholar]
- Etiology and outcome of crescentic glomerulonephritis. Indian Pediatr. 2013;50:283-8.
- [Google Scholar]
- Clinical spectrum and outcome of crescentic glomerulonephritis in children in developing countries. Pediatr Nephrol. 2008;23:389-94.
- [Google Scholar]
- The immunopathological spectrum of crescentic glomerulonephritis: A survey of 106 patients in a single Chinese center. Nephron Clin Pract. 2010;116:c65-74.
- [Google Scholar]
- Clinical spectrum of diffuse crescentic glomerulonephritis in Chinese patients. Chin Med J (Engl). 2003;116:1737-40.
- [Google Scholar]
- IgA nephropathy in a tertiary care center from south India. Indian J Nephrol. 2011;21:230-4.
- [Google Scholar]
- Primary immunoglobulin A (IgA) nephropathy in Western India. Indian J Nephrol. 2005;15:227-31.
- [Google Scholar]
- Clinicopathological characteristics and outcomes of patients with crescentic lupus nephritis. Kidney Int. 2009;76:307-17.
- [Google Scholar]
- Incidence and outcome of pauci-immune rapidly progressive glomerulonephritis in Wessex, UK: A 10-year retrospective study. Nephrol Dial Transplant. 2000;15:1593-9.
- [Google Scholar]
- Antineutrophil cytoplasmic autoantibody-negative pauci-immune crescentic glomerulonephritis. J Am Soc Nephrol. 2007;18:599-605.
- [Google Scholar]
- Anti-neutrophil cytoplasmic antibodies in 566 European patients with systemic lupus erythematosus: Prevalence, clinical associations and correlation with other autoantibodies. European Concerted Action on the Immunogenetics of SLE. Clin Exp Rheumatol. 1998;16:541-6.
- [Google Scholar]
- Anti-neutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus: Prevalence, clinical associations and correlation with other autoantibodies. J Assoc Physicians India. 2004;52:533-7.
- [Google Scholar]
- Necrotizing and crescentic lupus nephritis with antineutrophil cytoplasmic antibody seropositivity. Clin J Am Soc Nephrol. 2008;3:682-90.
- [Google Scholar]
- Analysis of risk factors for patient and renal survival in crescentic glomerulonephritis. Am J Kidney Dis. 1987;9:98-107.
- [Google Scholar]
- Poor renal outcome of antineutrophil cytoplasmic antibody negative Pauci-immune glomerulonephritis in Taiwanese. J Formos Med Assoc. 2006;105:804-12.
- [Google Scholar]
- Crescentic nephritis at Groote Schuur Hospital, South Africa – Not a benign disease. Clin Nephrol. 1994;42:22-9.
- [Google Scholar]
- Prediction of outcomes in crescentic IgA nephropathy in a multicenter cohort study. J Am Soc Nephrol. 2013;24:2118-25.
- [Google Scholar]
- Pathological spectrums and renal prognosis of severe lupus patients with rapidly progressive glomerulonephritis. Rheumatol Int. 2015;35:709-17.
- [Google Scholar]
- Clinical and histological outcome predictors in renal limited pauci-immune crescentic glomerulonephritis: A single centre experience. Int J Immunopathol Pharmacol. 2012;25:287-92.
- [Google Scholar]







