Translate this page into:
Swan-neck versus straight peritoneal dialysis catheter: Long-term effect on patient and method survival
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Peritoneal dialysis (PD) is limited mainly by a higher technique failure rate as compared to hemodialysis (HD), catheter malfunction being an important reason. Intra- and extra-peritoneal catheter configuration may be associated with mechanical and infectious complications affecting method survival. We report our experience with two extra-peritoneal catheter configurations: the straight and the swan-neck (SN) catheters. A total of 85 consecutive patients, 58 males and 27 females were included in the study. Among them, 26 were diabetics; 52 were treated with automated PD (APD) and 33 with continuous ambulatory PD (CAPD). Straight catheters were used in 38 patients (straight group) and SN catheters in 47 patients (SN group). Straight catheters were mostly used in the first 6-year period while SN catheters in the last 6-year period. The baseline demographics were similar between the two groups. A significantly higher frequency of APD use was observed in SN group. Technique survival was better with SN versus straight (log-rank test, P = 0.01) while patient and catheter survival were similar. A better technique survival is noted in our group of patients with SN catheters. An additional factor could be the significantly higher frequency of APD use in this group. Changes in PD solutions’ composition could also contribute to improvement in technique survival. The outcome for patients and catheter types used was similar.
Keywords
End-stage renal disease
outcomes
peritoneal catheter
peritoneal dialysis
survival
Introduction
Peritoneal dialysis (PD) as an alternative to hemodialysis (HD) is variably used for renal replacement therapy in patients with stage 5 chronic kidney disease who wait for or cannot receive a renal transplant. The relatively high technique failure rate, mainly due to PD catheter malfunction, is an important reason for PD lagging behind HD.[12] There are several variations of the PD catheter configuration that may be associated with mechanical and infectious complications and influence peritoneal access longevity. The most usual variations concern the intra-peritoneal segment (straight or coiled with and without discs), the subcutaneous/extra-peritoneal part (straight or swan-neck [SN]), and the number of cuffs (single or double). The benefit of one catheter over the other has not been conclusively demonstrated by comparative studies designed to evaluate the impact of different catheter configuration on technique complications.[3] In addition, most of the studies are underpowered by relatively short follow-up. Current clinical practice guidelines for peritoneal access do not clearly indicate the superiority of any particular design over the conventional straight Tenckhoff catheter.[14]
The aim of the present study was to evaluate retrospectively the impact of two extra-peritoneal catheter configurations, the straight and SN catheters, on technique, catheter and patient survival.
Subjects and Methods
We performed a retrospective analysis of all PD catheters that were inserted in our center between November 1993 and February 2013. Our study population comprised 85 consecutive patients, of which 58 were males and 27 were females with at least 3 months of follow-up, starting PD during the study period. Median age at PD initiation was 65 years (range: 21–91) and mean time of follow-up was 43.4 ± 31.3 months. Twenty-six patients were diabetics, 52 patients were treated with automated PD (APD), and 33 with continuous ambulatory PD (CAPD). Two different types of PD catheters were used throughout the study period: Double-cuff straight Tenckhoff catheter (Quinton Instrument Company, Seattle, WA, USA) and double-cuff SN catheter (Quinton Instrument Company, Bothell, WA, USA). The intra-peritoneal segment was straight in both types of catheters studied. The insertion of all catheters was performed by the same surgeon using laparoscopic surgical technique.
Patients were followed until death, renal transplantation, and transfer to other dialysis modality or another renal center. Survival curves (patient, technique, and catheter) were generated according to Kaplan–Meier method. Technique failure was defined as any situation where a patient on PD was transferred to HD for more than 3 months, excluding those patients that died, were successfully transplanted or recovered residual renal function.[5] Catheter failure was defined as removal of a dysfunctional PD catheter due to catheter-related complications. Log-rank test and χ2 were used for statistical analysis. The level of significance was set at P < 0.05.
Results
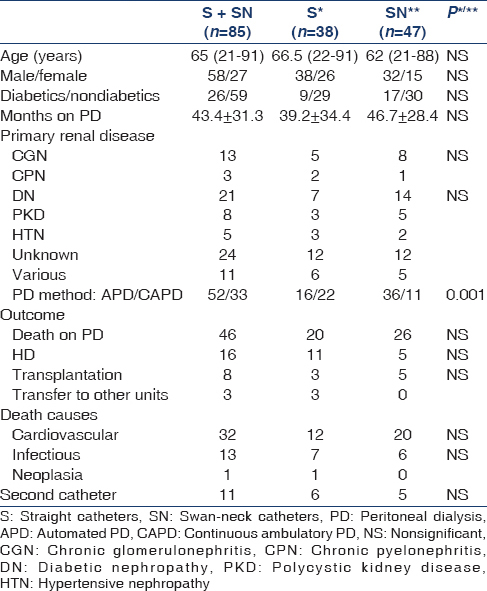
Straight catheters were used in 38 patients (straight group) and SN catheters in 47 patients (SN group). Straight catheters were mostly used in the first 6-year period while SN catheters in the last 6-year period. Demographic data for both groups are presented in Table 1. Baseline demographics were similar between the two groups. A significantly higher frequency of APD versus CAPD was observed in SN group. A second catheter was placed due to mechanical or infectious reasons in similar numbers in both groups.
Technique survival was significantly better in SN versus straight (log-rank test, P = 0.01) while patient and catheter survival were similar (P = 0.64 and P = 0.52, respectively). Catheter failure was noted in 11 patients, six of straight group and five of SN group due to mechanical (six patients) or infectious (five patients) complications. Kaplan-Meier curves for technique, patient, and catheter survival in both groups are shown in Figures 1–3, respectively.

- Technique survival in straight versus swan-neck catheters

- Patient survival in straight versus swan-neck catheters

- Catheter survival in straight versus swan-neck catheters
Discussion
A better technique survival was found in our group of patients with SN catheters compared to conventional straight ones. Patient and catheter survival rates were similar for both groups of different extra-peritoneal catheter design.
The potential influence of PD catheters’ extra-peritoneal configuration on long-term outcomes has not been adequately clarified so far. In a recent meta-analysis, 1-year and 2-year catheter survival between straight and SN PD catheters has been described in only four studies, two of which have been published before 2000, and no significant difference has been shown.[4] Similar results regarding shapes of the subcutaneous segment have been described in a previous meta-analysis as well.[6] However, the results of such meta-analyses should be interpreted with caution, mainly due to significant variations in methodologies and follow-up of the included studies. Indeed, local practices, and the length of follow-up are particularly important in comparing PD access outcomes.[7]
The only demographic difference between the two groups of our study was significantly higher frequency of APD use in SN catheters’ group. This may be a potential confounding factor in the better technique survival noted in SN catheters’ group. Unfortunately, in the above-mentioned meta-analyses,[46] data on PD submodality are lacking. Changes in PD solutions’ composition over the last few years and, in general, the improvements of overall practices in PD could also contribute to better technique survival observed in SN catheters group as these catheters have been increasingly used over the last decade in our unit. This is consistent with the observation made by many investigators that the more recent studies displayed better catheter survival rates compared with the older ones.[8] Our study demonstrated a benefit of SN over straight PD catheters regarding technique survival. However, this finding should be interpreted with caution due to the retrospective design of the study and the potential influence of many factors that our study was not appropriately designed to evaluate. The similar catheter survival rate demonstrated for both groups appears to be the only conclusive result.
Nevertheless, the type of peritoneal catheter is an important aspect regarding the outcome of PD. In the existing literature, there is no consensus about the type of catheter that is to be preferred for successful PD. However, it is generally accepted that PD catheter selection should be based on the individual patient's requirements as well as on local practices and experience.[18] Our study, despite the abovementioned limitations, evaluated the long-term effect of two different extra-peritoneal catheter designs on patient and technique survival and provides the rationale for large randomized trials to definitely address the important issue of the optimal PD catheter.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Changes in patient and technique survival over time among incident peritoneal dialysis patients in Canada. Clin J Am Soc Nephrol. 2012;7:1145-54.
- [Google Scholar]
- Noninfectious complications of peritoneal dialysis: Implications for patient and technique survival. J Am Soc Nephrol. 2007;18:3023-5.
- [Google Scholar]
- Peritoneal catheters and exit-site practices toward optimum peritoneal access: A review of current developments. Perit Dial Int. 2005;25:132-9.
- [Google Scholar]
- A systematic review and meta-analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney Int. 2014;85:920-32.
- [Google Scholar]
- Trends in patient and technique survival in peritoneal dialysis and strategies: How are we doing and how can we do better? Adv Ren Replace Ther. 2000;7:324-37.
- [Google Scholar]
- Coiled versus straight peritoneal dialysis catheters: A randomized controlled trial and meta-analysis. Am J Kidney Dis. 2011;58:946-55.
- [Google Scholar]
- Time-dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int. 2010;30:170-7.
- [Google Scholar]







