Translate this page into:
Hemodialysis outcomes and practice patterns in end-stage renal disease: Experience from a Tertiary Care Hospital in Kerala
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This study was planned to analyze the hemodialysis practice patterns from a tertiary care referral centre as there is very limited data from India. All patients of ESRD on maintenance hemodialysis (MHD) in dialysis unit at AIMS, Kochi, Kerala for a minimum period of 3 months were included. A total of 134 patients (M: F 2:1) with age of 20 to 84 years (Mean: 59.83; SD: 11.98) were studied. The most common causes of ESRD in study population were diabetic nephropathy (DN) (59.7%) followed by unclassified group (19.4%), chronic glomerulonephritis (CGN) (11.9%). Majority (81%) were initiated on MHD through temporary vascular access on emergency basis. Majority (79%) of the patients were on twice weekly MHD. The range of eGFR (ml/min/1.73 m2) at the time of initiation of MHD was 1.26-11.78 by CG formula and 2.18-16.4 by MDRD equation. The mean duration on hemodialysis was 37.16 months and 50.7% patients had died during the follow-up period (3-108 months). The mean survival time on hemodialysis was 40.31 months (SD = 26.69). The mean survival time was lower in diabetic nephropathy (35.93 months) than in non-diabetic renal disease (47.46 months). The most common causes of deaths were cardiovascular events (51.5%), and infections (26.5%). In conclusion, males outnumbered females, among those on hemodialysis. There was no significant difference in eGFR at initiation of MHD based on etiologies. Initiation of MHD via temporary access, presence of LVH, acute coronary syndrome, use of acetate dialysate, need for parenteral iron therapy had impact on mortality. Survival rates while on hemodialysis at end 1st, 3rd, 5th and 7th years were 87.31, 45.52, 21.64 and 7.46 percentages respectively.
Keywords
End-stage renal disease
hemodialysis
mortality risk factors
survival rate
Introduction
Dialysis therapy ameliorates many of clinical manifestations of end-stage renal disease (ESRD) and postpones imminent death. However, the hemodialysis patients have higher morbidity and mortality, multiple hospitalizations, unique treatment complications, such as vascular access failure, considerable expenses, and lower quality of life than the general population. The dialysis outcomes and practice patterns studies (DOPPS) which included patients from several countries (Japan, Australia, France, Germany, Italy, Spain, and the UK, the United States, Belgium, Canada and Sweden) with large populations of dialysis patients showed that dialysis practice varies widely among countries.[123] There are limited data regarding hemodialysis practice patterns from India.[45678] We did this study to document the clinical profile of patients on maintenance hemodialysis (MHD) in the dialysis unit at our hospital.
Materials and Methods
Patients of ESRD on MHD for a minimum period of 3 months in Dialysis unit, at Amrita Institute of Medical Sciences and Research Centre, Kochi were included in this retrospective study. Our Institute is one the premier tertiary referral Institutes in Kerala with all Specialty and Super specialty departments with the state of the art infrastructure and organ transplant program. The diagnosis of underlying kidney disease was based on clinical, laboratory and radiological features. Patients who were transferred to other units, patients switching to other forms of renal replacement therapy (RRT), those being evaluated for renal transplantation or on the waiting list with matched live related donor were excluded. The period of study was January 2003 to December 2011.
We recorded the patient age, gender, the cause of chronic kidney disease (CKD), comorbidities, estimated glomerular filtration rate (eGFR) at initiation hemodialysis, dialysis parameters (duration, frequency, vascular access), Erythropoietin use) survival on hemodialysis, causes of death. The mean of the 3-months value was analyzed for continuous variables.
Standard hemodialysis was performed for 5 h twice or 4 h thrice weekly. Individual proportioning dialysis machines were used with reverse-osmosis treated water. Volumetric ultrafiltration control was available in all the machines (Fresenius and B-Braun). Polysulfone hollow fiber dialyzers of mass transfer area co-efficient of 604-781 ml/min (Fresenius F HPS (High Performance; Steam Sterilized; 5/6/7) and ultrafiltration co-efficient 10–16 ml/h/mmHg (Fresenius F HPS 5/6/7) were used in all patients. Dialyzer surface area corresponding to 60% of BSA was selected for each patient. Dialysate flow rate was 500 ml/min and blood flow rates were targeted as per the patient requirement. Dialyzer re-use was uniformly performed using manual methods.
Statistical analysis
Mean ± standard deviation (SD) and percentages were used for summarizing the data. Relevant statistical tests were used for analysis of different variables. Continuous variables were studied using the Student's t-test. Categorical variables were analyzed using the Chi-square/Fisher's exact. The variables were also analyzed by multivariate analysis to assess their significance. The primary endpoint of the analysis was death. The confidence interval was 95%, and a two tailed P < 0.05 was used for statistical significance. All statistical analyses were performed with SPSS version 15.0: SPSS Inc., Chicago, IL, USA.
Results
A total of 134 patients (91 males) of ESRD on MHD who satisfied inclusion criteria were studied. The age of the patients ranged from 20 to 84 years (mean = 59.83 years, SD = 11.98 years). All patients were vaccinated for hepatitis B virus (HBV) and none of the patients had either HBV or hepatitis B virus (HCV) infection.
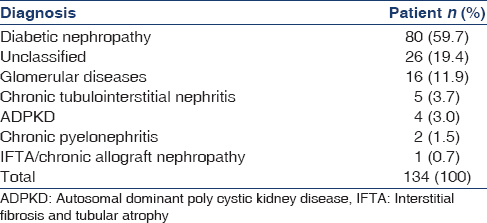
The most common cause of ESRD was diabetic nephropathy (DN) (59.7%) followed by unclassified group (19.4%), chronic glomerulonephritis (CGN) (11.9%) and others 9% (chronic interstitial nephritis, autosomal dominant polycystic kidney disease, chronic pyelonephritis and Interstitial fibrosis and tubular atrophy/chronic allograft nephropathy) [Table 1]. The most common causes of CGN were IgA nephropathy and focal segmental glomerulosclerosis followed by membranous nephropathy, amyloidosis, anti-glomerular basement membrane (GBM) antibody disease, and atheroembolic renal disease [Table 2]. The cause was undetermined in 19.4% of subjects as they presented with to the hospital with ESRD.

Majority of patients (81%) were initiated on hemodialysis through uncuffed dual lumen catheters (internal jugular vein in 66% and femoral vein in 15%) and arteriovenous fistula (AVF) was the vascular access in only 19% [Table 3]. Most of the patients (79%) were on twice-weekly hemodialysis (5 h each) and 21% were on thrice weekly (4 h each) sessions. Sixty-four percentage of patients were on acetate and 36% were on bicarbonate-based dialysate. The AVF was the permanent vascular access in the majority (87.3%) of patients, and 12.7% had cuffed catheter as an access (internal jugular catheter - 11.2% and femoral catheter - 1.5%) due to failed AVF [Table 3].

The mean eGFR at the time of initiation of MHD was 4.28 ml/min/1.73 m2 (Range - 1.26–11.78, SD = 1.94) by Cockroft-Gault formula and 5.71 ml/min/1.73 m2 (2.18–16.4, SD = 2.26) by MDRD equation. There was no statistically significant difference in eGFR at initiation of MHD based on etiologies for CKD (p = 0.09) [Table 4].

Hypertension (HTN) was the most common comorbidity (96.8%), followed by left ventricular hypertrophy (LVH) (80.6%), coronary artery disease (CAD) (52.3%), tuberculosis (11.6%), chronic liver disease (4.3%) and malignancies in 2.2% of patients [Table 5].

The mean duration on hemodialysis in the study was 37.16 months with a range of 3–108, and SD of 26.24 months. Sixty-eight (50.7%) out of the 134 patients had died during the above follow-up period. The mean survival time on hemodialysis was 40.31 months (SD = 26.69). The mean survival time was lower in DN (35.93 months) than in nondiabetic renal disease (47.46 months) was statistically significant (P < 0.05). The overall survival rates at end 1st, 3rd, 5th and 7th years were 87.31, 45.52, 21.64, and 7.46 percentages, respectively [Table 6 and Figure 1]. The survival rates were lower in those with DN than nondiabetic renal disease at each of the above time intervals, it was statistically significant (P < 0.05) [Table 6 and Figure 2].


- Survival graph of all patients

- Survival graphs: Comparison between diabetic chronic kidney disease and nondiabetic chronic kidney disease. (Curve 1: Diabetic chronic kidney disease, and Curve 2: Nondiabetic chronic kidney disease)
The hemoglobin level in patients on erythropoietin ranged from 9.7 to 12.3 g/dl (mean: 10) and it was 6.3–12.4 (mean: 9.6) g/dl in those on regular blood transfusions. The mean Erythropoietin dosage administered was 102.81 IU/Kg/week with a range from 4000 to10,000 IU/week (mean weight: 54.16 kg, mean erythropoietin dose: 5568.63 IU/week).
The most common causes of death the study were cardiovascular events (35, 51.5%), infections (18, 26.5%) followed by discontinuation of hemodialysis (2, 2.9%), advanced malignancy (2, 2.9%) and polytrauma following accident (1, 1.5%) and intracranial bleed (1, 1.5%), the cause was unknown in 13.2% (9) in cases. The numbers in brackets represent a number of patients and percentage contribution to all deaths. Acute coronary syndrome (26, 38.23%) was the most common cardiac cause of death followed by sudden cardiac death (SCD) (7, 10.29%), refractory ventricular arrhythmia (1, 1.5%) and cardiac amyloidosis (1, 1.5%). Most of the deaths due to SCD (6 out of 7) and all those due to unknown causes occurred at home. The SCD was presumed to be the cause as they had underlying CAD. However, an autopsy was not done, to confirm the etiology. The pneumonia was the most common (8; 11.6%) cause of infection-related deaths followed by catheter-related infections (4, 5.9%), cellulitis (4, 5.9%), pyogenic discitis (1, 1.5%) and disseminated varicella (1, 1.5%).
The age >50 years, the presence of LVH, CAD, anemia requiring multiple transfusions, parenteral iron therapy, hypoalbuminemia (<3.6 g/dl), initial temporary vascular access and duration on dialysis were shown to increase the risk of mortality statistically [Table 7]. Patients requiring multiple hospital admissions (>2, excluding those for initial evaluation or creation of AVF) had higher mortality (40.47%), than those needing <2 admissions 40.47% vs (14.63%, p = 0.008); statistically significant. The duration on MHD was the most important factor, affecting the mortality. Whereas as AVF as initial vascular access, appropriate correction of anemia with Erythropoietin had a favorable effect on survival [Table 7].

The presence of HTN alone did not affect mortality statistically (p = 0.62). However HTN requiring more than 3 drugs had an adverse effect on mortality (p = 0.04). Dialysis frequency (5 h twice a week or 4 h thrice week) and dialysate type (acetate or bicarbonate) did not statistically significant impact on mortality [Table 7].
Patient gender, serum calcium level, serum phosphorus level, calcium-phosphorus product, ferritin level and dialysis frequency did not have any statistically significant effect on mortality [Table 7].
On multivariate analysis initiation of MHD via temporary access (p = 0.034), presence of LVH (p: 0.029), acute coronary syndrome (p = 0.02), use of acetate dialysate (p = 0.006), need for parenteral iron therapy (p = 0.006) were shown to have statistically significant effect on mortality on multivariate analysis. Presence of HTN (p = 0.79), number of drugs need for its control (p = 0.642), hypoalbuminemia (p = 0.175), dialysis frequency (p = 0.832) did not have an effect on mortality on multivariate analysis.
Discussion
Males outnumbered females among those on MHD with M: F ratio of ~2:1 pattern consistent with DOPPS[1] and Indian studies[4567] in terms of age and sex ratios. In another study, the mean age was 38.6 years, with 22.8% of them undergoing renal transplantation.[5] Our study excluded those changing the mode of RRT to renal transplantation or chronic ambulatory peritoneal dialysis. Patients on waiting list for transplantation with eligible donors were also excluded thus explaining the older age of patients in the study.
The most common etiology for the ESRD in the study population was DN followed by unclassified group. The IgA nephropathy and focal segmental glomerulosclerosis were the 2 most common causes for biopsy proven glomerulopathies, followed by membranous nephropathy, amyloidosis, anti GBM antibody disease and atheroembolic renal disease. The etiologic pattern for ESRD as mentioned above, consistent with previous studies[46] and CKD registry of India.[7] The DN as etiologic factor was more common in the study group in comparison to earlier studies (29.2–44.7%),[467] as those with other etiologies are relatively younger and undergo transplantation, which were excluded from our study.
In our study, the majority of patients were initiated on hemodialysis through uncuffed dual lumen catheters only minority having mature AVF at the time of presentation to Nephrologist, a consistent finding noted in other studies.[67] The majority of patients required emergency hemodialysis and the internal jugular catheter was the most common form of vascular access at the initiation of hemodialysis in our study consistent with previous reports.[68] AVF was present only in minority of patients at presentation similar to previous studies.[678] This is due to treatment of CKD with conservative measures until late stages without the timely creation of AVF by primary care Physician or treatment at a peripheral center without facilities for vascular surgery or lack of knowledge regarding the timing of AVF creation.[791011]
The AVF was the permanent vascular access in the majority of patients while on MHD and most of the patients were on twice weekly hemodialysis, similar to an earlier study.[4]
Theoretical considerations support initiation of dialysis therapy at a GFR of approximately 10–15 mL/min/1.73 m2, and this was the recommendation of the Kidney Disease Outcomes Quality Initiative-Hemodialysis-1997 (KDOQI HD) adequacy guideline. In one the earlier studies dialysis therapy was in initiated at mean eGFR of 9.8 mL/min/1.73 m2, with lower range for a range of 7–9 for young and middle-aged adults and 10–10.5 mL/min/1.73 m2 for children and elderly patients.[12] The mean eGFR at the time of initiation of MHD in the present study was 4.28 ml/min/1.73 m2 by Cockroft-Gault formula and 5.71 ml/min/1.73 m2 by MDRD equation. There was no statistically significant difference in eGFR at initiation of MHD based on etiologies for CKD. We have not assessed the difference eGFR based on age in the present study. However, registry data from the USA, Canada, and the UK show that patients with comorbidities initiate dialysis therapy at higher levels of eGFR.[121314] There is no previous Indian data regarding eGFR at initiation of dialysis therapy.
The HTN was the most common comorbidity followed by, LVH, CAD and tuberculosis. The majority of the patients had lower hemoglobin level in the study as against the recommended target of 11–12 g/dl as per KDOQI, consistent with the earlier study.[4] Cardiovascular disorders and anemia are very common comorbidities in ESRD consistent with their description in literature.[1516]
The survival on hemodialysis was inversely proportional to time on dialysis. The US Renal Data System data (2012), showed a similar trend with time on dialysis, with survival rates at 1st, 5th, and 10th years of 77, 22, and 12 percentages, respectively.[17] The survival rates were significantly lower in those with DN than nondiabetic renal disease at each of the above time intervals in our study, consistent an earlier report.[18]
The two most common causes of deaths were cardiovascular events and infections, followed unknown causes, discontinuation of hemodialysis, advanced malignancies, polytrauma following the accident and intracranial bleed. Acute coronary syndrome was the most common cardiac cause of death followed by sudden cardiac death, refractory ventricular arrhythmia, and cardiac amyloidosis. Pneumonia was the most common cause of infection-related deaths followed by catheter related infections, cellulitis, pyogenic discitis, and disseminated varicella. Infections followed by ischemic heart disease, inadequate hemodialysis, withdrawal from dialysis were reported as the causes of death in an earlier study.[4] The vascular access-related infections (abscess of the AVF and catheter-related bacteremia) were the most common cause of sepsis in one the study[4] and most common being urinary tract infections in another study.[6] In a study from the USA; cardiovascular events most common cause of mortality followed by infectious, similar to the present study.[19]
Age >50 years, LVH, CAD, anemia requiring multiple transfusions, hypoalbuminemia (<3.6 g/dl), initial temporary vascular access, use of acetate dialysate and duration on dialysis were shown to increase the risk of mortality statistically. The duration on MHD was the most important factor, affecting the mortality. Hypoalbuminemia was shown to increase the mortality risk in previous studies.[3420] The albumin level used for defining hypoalbuminemia varied in studies <4.0 g/dl in one[20] and <3 g/dl in another;[4] <3.6 g/dl was used in the present study. The need for parenteral iron therapy in comparison to oral iron therapy also increased the mortality risk significantly.
Age <50 years, AVF as initial vascular access, appropriate correction of anemia with erythropoietin had a favorable effect on survival, consistent with earlier reports, emphasizing the importance of the creation of AVF at the appropriate time during treatment of CKD.[91011] The use of erythropoietin shown improve the quality of life, in several a meta-analysis,[2122] however, the effect on survival is less clear, necessitating for multicenter trials to assess its effect on Indian population. In one of the single center studies, use of erythropoietin did not affect survival on dialysis.[4]
The presence of HTN alone did not affect mortality statistically; however, HTN requiring more than three drugs had an adverse effect on mortality. The gender, serum calcium, serum phosphorus, calcium-phosphorus product, ferritin, dialysis frequency (5 h twice a week or 4 h thrice week) did not have any statistically significant effect on mortality in our study. An earlier study also showed that HTN, type of native kidney disease, hemoglobin level, the calcium-phosphorus product had no significant effect on the outcome.[4] Diabetes nephropathy as native kidney disease increased the mortality risk in our study, consistent with previous reports.[2324]
Initiation of MHD via temporary access, the presence of LVH, acute coronary syndrome, use of acetate dialysate, need for parenteral iron therapy had statistically significant mortality on multivariate analysis. Whereas, the presence of hypoalbuminemia, HTN and dialysis frequency (4 h 3 times/week or 5 h 2 times/week), did not have any statistically significant effect on mortality.
Limitations of the study
This being a single center study the results may not be generalized, highlighting the need for multicenter trial with the uniform protocol. The effect of interdialytic weight gain was not studied. Our study did not have patients with HBV or HCV infection to assess their impact on mortality. The erythropoietin resistance and its impact on mortality were not assessed. Dialysis adequacy or residual renal function was not estimated in the study; however, there was no statistically significant difference mortality between twice weekly dialysis (total of 10 h) and thrice weekly (total of 12 h) schedule.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: The dialysis outcomes and practice patterns study (DOPPS) PLoS Med. 2014;11:e1001750.
- [Google Scholar]
- Practice-based versus patient-level outcomes research in hemodialysis: The DOPPS (Dialysis Outcomes and Practice Patterns Study) experience. Am J Kidney Dis. 2014;64:969-77.
- [Google Scholar]
- Independent and joint associations of nutritional status indicators with mortality risk among chronic hemodialysis patients in the dialysis outcomes and practice patterns study (DOPPS) J Ren Nutr. 2010;20:224-34.
- [Google Scholar]
- Survival analysis of patients on maintenance hemodialysis. Indian J Nephrol. 2014;24:206-13.
- [Google Scholar]
- Haemodialysis for end-stage renal disease in Southern India – A perspective from a tertiary referral care centre. Nephrol Dial Transplant. 1998;13:2494-500.
- [Google Scholar]
- End-stage renal disease patients on hemodialysis: A study from a tertiary care center in a developing country. Hemodial Int. 2011;15:312-9.
- [Google Scholar]
- What do we know about chronic kidney disease in India: First report of the Indian CKD registry? BMC Nephrol. 2012;13:10.
- [Google Scholar]
- Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol. 1999;10:1281-6.
- [Google Scholar]
- Timing of nephrologist referral and arteriovenous access use: The CHOICE study. Am J Kidney Dis. 2001;38:494-501.
- [Google Scholar]
- Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J Clin Epidemiol. 2002;55:711-6.
- [Google Scholar]
- Bethesda. US Renal Data System: USRDS 2004 Annual Data Report. The National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases 2004
- Canadian survey of clinical status at dialysis initiation 1998-1999: A multicenter prospective survey. Clin Nephrol. 2002;58:282-8.
- [Google Scholar]
- The Renal Association UK Renal Registry. The Sixth Annual Report 2003
- Cardiovascular Disease in Chronic Kidney Disease in Comprehensive Clinical Nephrology (4th ed). Missouri: Elsevier Saunders; 2010. p. :935-50.
- Anemia in Chronic Kidney Disease in Comprehensive Clinical Nephrology (4th ed). Missouri: Elsevier Saunders; 2010. p. :951-8.
- Dialysis and Transplant: Patient Survival Statistics. End-Stage Renal Disease in the United States. Annual Report of U.S. Renal Data System (USRDS) 2012
- Survival of end-stage renal disease diabetic patients on hemodialysis. Hemodial Int. 2004;8:87-8.
- [Google Scholar]
- United States Renal Data System. Excerpts from USRDS 2008 Annual Data Report. U.S. Department of Health and Human Services. The National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Am J Kidney Dis. 2009;53:S47-S64. DOI: http://dx.doi.org/10.1053/j.ajkd. 2008.10.014
- [Google Scholar]
- Are nutritional status indicators associated with mortality in the hemodialysis (HEMO) study? Kidney Int. 2005;68:1766-76.
- [Google Scholar]
- Hemoglobin targets for the anemia of chronic kidney disease: A meta-analysis of randomized, controlled trials. J Am Soc Nephrol. 2004;15:3154-65.
- [Google Scholar]
- Impact of epoetin alfa on clinical end points in patients with chronic renal failure: A meta-analysis. Kidney Int. 2004;65:757-67.
- [Google Scholar]
- Diabetes: Changing the fate of diabetics in the dialysis unit. Blood Purif. 2007;25:39-47.
- [Google Scholar]







