Translate this page into:
An Unusual Association of Renal Cell Carcinoma and Renal Malakoplakia with Focal Segmental Glomerulosclerosis in an Elderly Patient
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The association of malignancy and glomerulonephritis may be missed, especially in elderly patients. Here, we report a case of eosinophilic variant of renal cell carcinoma and renal parenchymal malakoplakia discovered on renal biopsy in a patient with steroid-dependent nephrotic syndrome. The presence of malakoplakia in our biopsy was probably due to systemic steroid therapy for glomerulonephritis, presence of concomitant asymptomatic urinary tract infection, and/or history of diabetes mellitus. The patient had remission of proteinuria following laparoscopic removal of the tumor, indicating probable remission of glomerulonephritis.
Keywords
Focal segmental glomerulosclerosis
malakoplakia
renal cell carcinoma
Introduction
Chronic kidney disease with preceding glomerulonephritis in the elderly may still benefit from a renal biopsy for appropriate diagnosis, management, and prognostication.[1] Many a times, a biopsy is not performed, and it is treated empirically. Search for secondary causes of nephrotic syndrome is mandatory before steroid therapy. The association of malignancy and glomerulonephritis may be missed unless detailed evaluation is undertaken in the older population.[2] Other comorbid conditions such as hypothyroidism, diabetes mellitus, and hypertension may increase the threshold for doing a biopsy. The association of focal segmental glomerulosclerosis (FSGS), renal cell carcinoma (RCC), and renal parenchymal malakoplakia has not been reported previously.
Case Report
A female patient aged 65 years with Type 2 diabetes mellitus, hypothyroidism, and hypertension came to our center with edema and was detected to have 4+ albumin on urine dipstick and proteinuria of 3.8 g/day. Her serum creatinine was 1.1 mg/dl and serum albumin was 2.5 g/dl. One year ago, she was diagnosed elsewhere as minimal change disease (MCD) following a kidney biopsy, for which she was given oral prednisone, which had resulted in partial remission. At our center, she was reinitiated on 1 mg/kg/day of prednisone and had partial remission at 12 weeks to 1.2 g/day. However, when we started tapering her steroids, her proteinuria increased to nephrotic range. She continued to take thyroid replacement therapy. She also complained of anorexia, weight loss, and fever. Secondary workup was redone, and her viral markers, antinuclear antibody serology, serum protein electrophoresis, and stool occult blood were all negative. She had pallor, blood pressure was 120/80 mmHg, heart rate was 97 bpm, and body mass index was 17 kg/m2. The systemic examination was otherwise unremarkable. She had no costovertebral angle tenderness. Urine analysis showed dipstick albuminuria of 3+ with many white blood cells, granular casts, and no hematuria. Other investigations showed hemoglobin of 9 g/dl, erythrocyte sedimentation rate of 126 mm at 1 h, serum creatinine of 0.7 mg/dl, and serum albumin of 3 g/dl. Urine culture showed no growth. We tapered her steroids to 5 mg/day and stopped it gradually.
We decided to rebiopsy her as she was steroid dependent and had some secondary characteristics. Incidentally, we found a 1.5 cm × 1.5 cm mass on the left kidney which was not reported previously. The renal biopsy revealed FSGS, tip variant [Figure 1a] with an area showing sheets of large polygonal cells with eosinophilic granular cytoplasm and small round-to-oval nucleus with distinct nucleolus, suggestive of RCC [Figure 1b]. A positron emission tomography (PET) - computed tomography scan was performed which revealed a metabolically active mass in the left kidney [Figure 2], left para-aortic nodal enlargement at the same level, and two small cavitary lesions in the right lower lobe of the lung [Figure 2]. The sputum examination was negative for malignancy and infection. A formal diagnosis of RCC was made, and laparoscopic left radical nephrectomy was done. The cut-section of the kidney revealed a circumscribed, tan-colored lesion with purulent necrotic material at the mid pole. The necrotic material involved the capsule of the kidney. Microscopic examination showed sheets of similar cells as described in the biopsy. At foci, loose clusters of macrophages with Michaelis–Gutmann bodies were seen [Figure 1c]. Immunohistochemistry markers vimentin, CD-10, epithelial membrane antigen, and CD-68 were strongly positive. A diagnosis of eosinophilic variant of conventional RCC with incident malakoplakia was made. Repeat urinalysis 4 weeks post surgery was negative for dipstick protein and a protein creatinine ratio of 0.6 mg/g [Figure 1d].
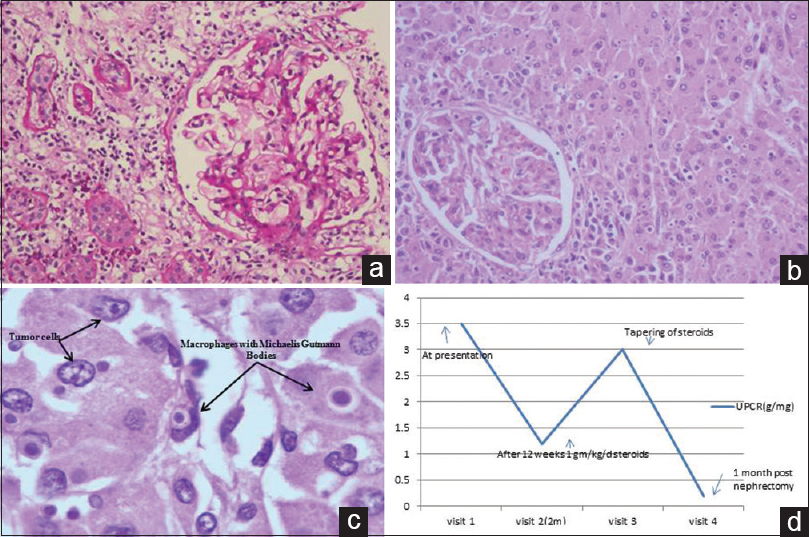
- (a) Tip variant focal segmental glomerulosclerosis (PAS, ×200), (b) sheets of tumor cells (large polygonal) surrounding a glomeruli (H and E, ×200), (c) Michaelis–Gutmann bodies (H and E, ×400). Immunohistochemistry markers vimentin, CD-10, epithelial membrane antigen, and CD-68 were strongly positive. (d) Graph showing the trend of proteinuria before and after nephrectomy

- Positron emission tomography-computed tomographic image showing metabolically active mass in the left kidney and active cavitary lesions in the lower lobe of the right lung
Discussion
Solid tumors can be associated with paraneoplastic glomerulonephritis which may include membranous nephropathy, MCD, FSGS, membranoproliferative glomerulonephritis, rapidly progressive glomerulonephritis, and IgA nephropathy.[3] In the case of membranous nephropathy, the diagnosis of paraneoplastic glomerulonephritis may precede cancer diagnosis by 1 year.[3] Elderly patients with glomerulonephritis should be thoroughly evaluated for potential underlying diseases, especially when atypical features such as weight loss, anorexia, lymphadenopathy, acute renal dysfunction, or incomplete remission with treatment are present. One should be vigilant in investigating older age group population with a glomerular disease for underlying malignancy. When fever of unknown etiology is present in association with a renal mass, the possible differential diagnosis includes RCC, malakoplakia, renal tuberculosis, and xanthogranulomatous pyelonephritis.[4] To the best of our knowledge, RCC with associated malakoplakia is extremely rare with only one reported case.[5] The presence of malakoplakia in our biopsy was probably due to systemic steroid therapy for glomerulonephritis and/or history of diabetes mellitus.[6] The remission of the albuminuria following removal of the tumor within a short span suggests the impact of tumor removal on secondary glomerular podocytopathy. With advances in technology, it raises the question whether one should advocate the use of a PET scan in an elderly patient with glomerular disease. The patient moved to another state and is being followed up there.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Secondary minimal change disease. Nephrol Dial Transplant. 2003;18(Suppl 6):vi52-8.
- [Google Scholar]
- Pathogenesis, diagnosis and management of paraneoplastic glomerulonephritis. Nat Rev Nephrol. 2011;7:85-95.
- [Google Scholar]
- Fever of unknown origin (FUO) and a renal mass: Renal cell carcinoma, renal tuberculosis, renal malakoplakia, or xanthogranulomatous pyelonephritis? Heart Lung. 2012;41:606-9.
- [Google Scholar]







