Translate this page into:
Study of FGF 23 Levels in Patients with Acute Kidney Injury and its Outcome
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
FGF23 has been proposed to be a putative marker of AKI severity and correlates positively with increased in-hospital adverse outcomes including need for renal replacement therapy (RRT) and death.[1] However, long-term effects of FGF23 in AKI including subsequent progression to CKD require further deliberation.[2] In this context, we hypothesized whether higher FGF23 at the outset in dialysis-requiring AKI patients is associated with increased risk of progression to CKD and mortality at 3 months.
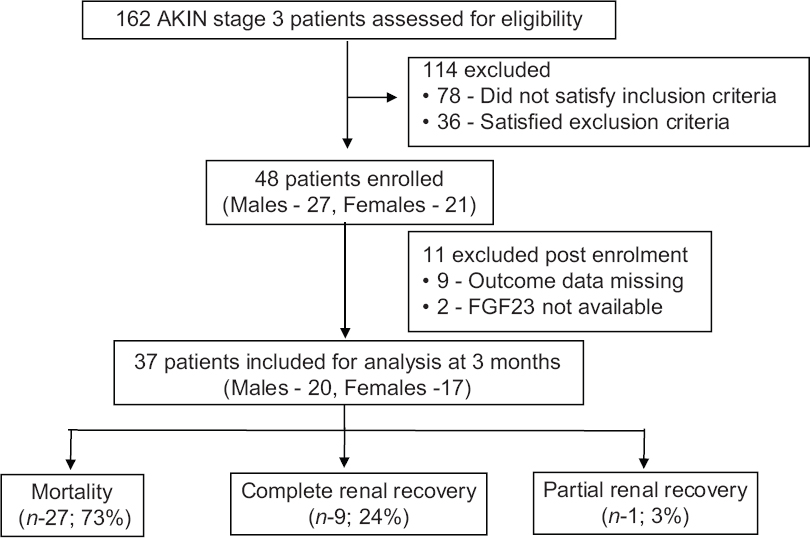
The study was a prospective, observational trial conducted at PGIMER, Chandigarh, India. Admitted patients with AKI (severity based on AKIN staging) were eligible for screening. Inclusion criteria were age between 18 and 75 years and AKIN stage 3 AKI requiring RRT. Exclusion criteria were suspected/known diagnosis of CKD, parathyroid disease, metabolic bone disease, history of gastrointestinal surgery, and renal or extrarenal conditions for which immunosuppressive therapy was contemplated. About 162 patients were assessed for eligibility; however, 48 patients satisfying both inclusion and exclusion criteria were enrolled [Figure 1] and 37 patients qualified for analysis. The study population was homogenous with respect to the mode of RRT with all receiving SLED.
- Study design and outcome of patients
Samples for calcium, phosphate, iPTH, 25OH Vitamin D, and FGF23 were drawn (just before the first dialysis) at enrolment. Samples for FGF23 were centrifuged, aliquoted and stored at −80°C, and measured by second generation ELISA. Patients were closely monitored during hospital stay and followed up after discharge at 2 weekly intervals till 3 months for clinical endpoints (recovery of renal function or death).
Etiology of AKI and baseline characteristics of the study cohort is depicted vide Table 1. By third month, 27 (73%) patients expired; 25 (68%) during the same admission, and 2 (5%) died within 3 months of discharge. Out of 10 patients alive at the end of 3 months, 9 (90%) had complete renal recovery, whereas 1 (10%) had partial renal recovery; with serum creatinine of 1.5 mg/dL (eGFR- 45 mL/min by MDRD-6 variable equation). Patients who died during the study period had significantly higher FGF23 compared with patients who survived [14.37 (IQR, 4.82–60.00) vs. 4.65 (IQR, 4.31–8.18); P = 0.039]. Accuracy of FGF23 in predicting death was fair (AUC = 0.733); with cutoff at 22.77 pg/mL, mortality prediction had sensitivity and specificity of 70% and 78%, respectively.
| Etiology of AKI in study participants | |
|---|---|
| 1. Medical AKI | n=36 (75%) |
| Sepsis induced | 23 (64%) |
| Type 1 hepatorenal syndrome | 4 (11%) |
| Tropical febrile illnesses | 4 (11%) |
| Hemotoxic snake envenomation | 3 (8%) |
| Acute diarrheal illness | 2 (6%) |
| 2. Surgical AKI | n-6 (12.5%) |
| Perforation peritonitis | 1 (2%) |
| Postoperative sepsis | 5 (10%) |
| 3. Obstetric causes | n-6 (12.5%) |
| Antepartum hemorrhage | 2 (4%) |
| Postpartum hemorrhage | 1 (2%) |
| Eclampsia | 3 (6%) |
| Baseline characteristics of the study participants | |
| Parameters | Cases (n=48) |
| Age (years) | 39.65 15.69 (18-74 years) |
| Sex | 27 males/21 females |
| APACHE II* | 21 (IQR, 12-26) |
| Creatinine (mg/dL) | 5.77±3.14 mg/dL (range, 1.6-14.7) |
| Corrected calcium | 8.90 (IQR, 8.28-9.66) mg/dL |
| Phosphorus | 4.50 (IQR, 3.25-5.50) mg/dL |
| 25 (OH) Vitamin D | 3.91 (IQR, 3.60-14.73) ng/mL |
| iPTH** | 52.10 (IQR, 22.43-111.48) pg/mL |
| S albumin | 2.30 (IQR, 1.95-2.60) g/dL |
| FGF23*** | 14.37 (IQR, 4.82-60.00) pg/mL |
*Acute physiology and chronic health evaluation, **Intact parathyroid hormone, ***Fibroblast growth factor 23
Septic AKI is recognized to be clinically and pathophysiologically distinct from non-septic AKI with a greater need for mechanical ventilation and higher mortality. Patients with septic AKI although euvolemic at presentation require RRT later in the course of hospital stay, however have faster dialysis independence than their non-septic counterpart,[3] possibly explained by hibernating renal tubular cells as apoptosis[4] and necrosis is distinctly less common in septic AKI.
Mortality (73%) in index study although high, nevertheless is comparable to national[5] as well as international studies[3] possibly due to referral bias of critically ill patients to tertiary care hospital and sepsis was the most frequent cause of AKI. Likewise renal recovery at 3 months was observed in 10 patients only (27%).
Factors which may directly influence both FGF23 and mortality include, AKI severity, disease severity, and sepsis. As all the participants in the present study had AKIN stage 3 AKI, the severity of AKI probably cannot explain the link between FGF23 and mortality. Likewise, sepsis was also not more frequent in the study participants who succumbed to their illness as compared to survivors (40% vs. 44%), and hence, severity of underlying illness probably remains the most likely explanation for increased mortality with high FGF23. As expected the APACHE score of the non-survivor group was significantly higher than that of the survivor group (21.50 ± 6.28 vs. 10 ± 7.56; P = 0.005). Both the groups had mostly similar burden of comorbidities (survivors vs. non-survivors (hypertension = 1/10 vs. 2/27, malignancy = 1/10 vs. 2/27, ischemic heart disease = 1/10 vs. 0/27, chronic liver disease = 1/10 vs. 3/27)).
Limitations of our study include small sample size (complete data was available for only 37 out of 48 patients enrolled). Besides, as most of the patients were recruited from January to April (before onset of monsoon in India with its attendant rise in vector-borne diseases), hence it does not capture full spectrum of community-acquired AKI. Samples for FGF23 were collected at enrollment only; further samples at least monthly would have helped us in analyzing the relationship between FGF23 change and renal recovery. Last, the instability of iFGF23 might have confounded the results. Smith et al.[6] have demonstrated that within 30–120 min of sample collection, iFGF23 undergoes significant but variable degradation leading to loss of immunoreactivity, and fate of iFGF23 stored at −80°C is unknown.
The study concludes that patients with dialysis-requiring AKI have higher mortality and FGF23 levels at the outset predict death with reasonable accuracy. Nevertheless, recovery from the acute illness ensures renal recovery in majority.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- FGF-23 levels inpatients with AKI and risk of adverse outcomes. Clin J Am Soc Nephrol. 2012;7:1217-23.
- [Google Scholar]
- Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 2012;81:442-8.
- [Google Scholar]
- Septic acute kidney injury in critically ill patients: Clinical characteristics and outcomes. Clin J Am Soc Nephrol. 2007;2:431-9.
- [Google Scholar]
- A unified theory of sepsis-induced acute kidney injury: Inflammation, microcirculatory dysfunction, bioenergetics, and tubular cell adaptation to injury. Shock (Augusta, Ga). 2014;41:3-11.
- [Google Scholar]
- Septic acute kidney injury in critically ill Indian patients. Indian J Crit Care Med. 2013;17:49-52.
- [Google Scholar]
- Instability of fibroblast growth factor-23: Implications for clinical studies. Int J Clin Chem. 2011;412:1008-11.
- [Google Scholar]






