Translate this page into:
Postinfectious glomerulonephritis: Is there a role for steroids?
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The role of steroids in treatment of postinfectious glomerulonephritis (PIGN) has been controversial. The reason for such controversy is the risk of infection relapse associated with steroid therapy. Steroids may have a place in the treatment of resistant cases where renal function does not improve despite aggressive antibiotic therapy as well as in patients with crescentic form of PIGN. We report a case of a 39 year-old Caucasian man who was diagnosed with methicillin-resistant Staphylococcus aureus (MRSA) bacteremia resulting in acute IgA dominant PIGN that failed to respond to antibiotic treatment alone, but responded significantly to steroids in addition to antibiotics. This anecdotal experience suggests that steroids could be considered in conjunction with antibiotic therapy for the treatment of refractory cases of PIGN or crescentic form of PIGN. More studies with long-term follow-up of patients treated with steroids in addition to antimicrobial agents are required to quantify the risk of infection relapse with steroid therapy.
Keywords
Methicillin-resistant Staphylococcus aureus
postinfectious glomerulonephritis
postinfectious glomerulonephritis
steroids
Introduction
Glomerulonephritis occurring as a consequence of MRSA infection was first reported by Koyama in 1995.[1] Subsequently more cases were reported that elaborated the histopathology and pathogenesis including role of Staphylococcal cell envelope antigen.[2–4] However, there are only a few case reports that focus on the treatment of this entity. The roles of steroids have been controversial with regard to their indications, timing and long-term complications including relapse of infection.[56] We report a case of post-MRSA IgA dominant PIGN that required treatment with steroids in addition to antibiotic therapy.
Case Report
A 39 year-old Caucasian man was transferred from an outlying facility for management of a psoas abscess diagnosed on computerized tomography (CT) scan of abdomen and pelvis. He complained of low back pain for 2 weeks. He denied any fever, trauma, tingling, numbness, bladder, or bowel disturbances. Past medical history was unremarkable except for an abscess on his right forearm and right scrotal area following a tick bite which was draining a couple of days before he started having back pain. Physical exam revealed tachycardia, tachypnea and minimal costovertebral angle tenderness bilaterally. Rest of the physical exam including neurological exam was within normal limits. Laboratory data revealed white blood cell count 33.8 thousand/mm3 (neutrophils count 31,900/mm3 and bands 24%), hemoglobin 11.9 gm/dl, sodium 124 mmol/l, potassium 4.5 mmol/l, blood urea nitrogen 24 mg/dl, creatinine 1.1 mg/dl, total protein 7.3 gm/dl, albumin 1.5 gm/dl. Urinalysis was significant for small amount of blood, red blood cells (8/hpf), white blood cells (10/hpf) and occasional white blood cell casts. Urine color, specific gravity and PH were within normal limits.
A CT scan of the abdomen without contrast done at an outlying facility revealed possible psoas abscess and left renal abscess [Figure 1]. Magnetic resonance imaging (MRI) of the lumbar spine confirmed the findings including multiple abscesses in the psoas muscles bilaterally and spondylitis involving L1–L4. CT guided biopsy of the left paravertebral mass as well as blood culture grew MRSA. Patient was started on vancomycin and levofloxacin with a plan to continue these antibiotics for at least 4–6 weeks.

- CT scan of abdomen with contrast showing bilateral psoas abscesses
During the hospital course, his condition started improving clinically; however his renal function started deteriorating and he developed acute renal failure. His blood urea nitrogen and creatinine increased from a baseline of 12 mg/dl and 1.1 mg/dl, respectively, to 24 and 2.4 mg/dl within 20 days of hospitalization and these values continued to increase. Within the next 2 weeks his blood urea nitrogen and creatinine were increased to 43 and 7.4 mg/dl, respectively. After 2 weeks of antibiotic treatment urine output decreased significantly. He was started on hemodialysis as he developed volume overload. Vancomycin and levofloxacin were stopped and the patient was started on linezolid, which also was stopped after six days as the patient developed an apparent allergic skin reaction. He was then started on daptomycin. The time course of serum creatinine is shown in Figure 2.

- Serum creatinine time course and antibiotics administered during the hospital stay
During this time period patient was evaluated for the cause of acute renal failure. His urine analysis at this point revealed red blood cells 56/hpf, a few dysmorphic red blood cells, WBCs <1/hpf, no eosinophils, proteinuria with urine protein to creatinine ratio 2.94, fractional excretion of sodium 7.67, and fractional excretion of urea 124.5; urine microscopic exam revealed few muddy brown casts. The urine color was brown and specific gravity was normal. His renal function did not return to baseline after a few days of hemodialysis. Considering the possibility of acute glomerulonephritis, the patient underwent CT guided biopsy of the right kidney, which revealed IgA dominant PIGN with extensive acute tubular injury and acute interstitial nephritis. Light microscopy showed glomeruli with mild to moderate increase in the mesangial matrix and cellularity, with cellular crescents in 2 of the 3 glomeruli sampled, and fibrinoid necrosis in one of these. In addition, rare hump shaped deposits were visualized overlying the glomerular basement membrane in the capillary notch area [Figure 3a]. Correspondingly, immunofluorescence (IF) microscopy showed 2+ mesangial and segmental capillary loop staining for IgA and C3 while IgG was negative [Figure 3b]. Electron microscopy showed scattered mesangial deposits and rare subepithelial hump type deposits [Figure 3c]. These findings were characteristic of IgA dominant postinfectious glomerulonephritis. The biopsy also showed acute tubular injury and a hypersensitivity drug induced acute interstitial nephritis, with widespread tubultitis and interstitial nephritis in areas away from the crescents.
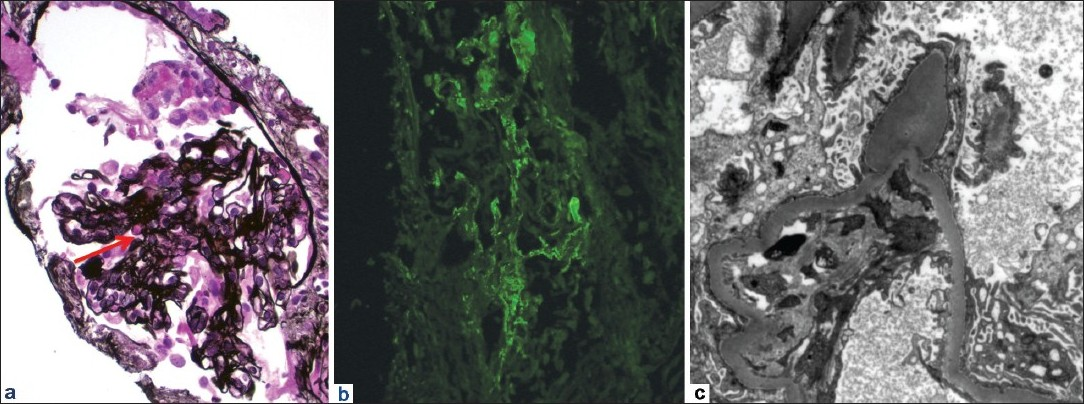
- (a) Glomerulus with small cellular crescent, fibrinoid necrosis (top) and small hump-shaped deposit (arrow) (Jones’ silver stain, ×400). (b) Immunofluorescence showed 2+ IgA predominantly mesangial and segmental capillary wall staining (anti-IgA IF, ×400). (c) By electron microscopy, rare hump-type subepithelial deposits were seen, protruding out from the basement membrane, in addition to scattered mesangial deposits (transmission electron microscopy, ×10,000)
The patient received pulse doses of steroids followed by oral steroids. He was discharged with arrangements to receive intravenous antibiotics and hemodialysis. His creatinine at the onset of the steroid therapy was 5.5 mg/dl, which improved after 2 weeks of treatment, at which point he was removed off hemodialysis. On follow up at three months and at one year, his creatinine was 1.7 and 1.3 mg/dl, respectively.
Discussion
Post-MRSA infection glomerulonephritis has been well documented in Japan. However, as the incidence of MRSA infection increases globally and the association between MRSA infection and IgA dominant glomerulonephritis is now clear, more cases are being reported from all countries including the United States. Clinical manifestations of PIGN following MRSA infection include acute renal failure developing within 4–10 weeks after the onset of infection.[5] Kidney biopsy should be considered in all patients with ARF and documented infection when PIGN is suspected to confirm the diagnosis and determine the need for steroid therapy especially when renal function does not improve with antibiotic treatment as patients with presence of crescents on renal biopsy usually require treatment with steroids. It may be difficult to differentiate PIGN from IgA nephropathy. In classic acute PIGN cases, there is an acute exudative proliferative response with frequent polymorphonucler leucocytes (PMNs) infiltrating the glomeruli. In more chronic cases, there is less PMN infiltration. Electron microscopy can then be helpful in demonstrating the typical subepithelial humps characteristic of postinfectious glomerulonephritis, contrasting the lack of such deposits in usual IgA nephropathy.[4] The coexisting AIN may also have contributed to renal dysfunction, as in our patient. In such instances it is always difficult to quantify the response obtained in terms of improvement in renal function with respect to different disease processes affecting the kidneys.
There have been case reports of successful treatment of PIGN following MRSA infection with antimicrobial agents only.[67] A study done in Japan included eight patients; six of which were treated with antibiotics only and the rest of the patients received steroids.[6] The patients who received steroids only had poor outcome secondary to relapse of the infection. Two of the six patients who received steroid therapy were diagnosed after five months and three months of their presentations, respectively, and were not on antibiotic treatment when they received steroid therapy. As these patients developed glomerulonephritis a few months after the initial infection, it may be possible that these patients had persistent MRSA activity. The patients, who were treated with antibiotics only, responded very well. Therefore, these cases do not reflect the refractory cases that fail to respond to antimicrobial agents only. On the other hand, there are several case reports of successful treatment of resistant cases of PIGN following MRSA infection with steroids without any relapse of the infection.[78] The role of steroids in these patients could be explained by the pathogenesis of PIGN, which involves the interaction of the host immune system with bacterial superantigen.
Based on our experience, we would like to suggest a possible role of steroid therapy in PIGN who fail to respond to antibiotic therapy alone and in patients with crescentic form of PIGN. It is also possible that the presence of AIN contributed to steroid responsiveness in our patient. The benefits of steroid therapy in terms of impact on quality of life may be considered significant as it may alleviate the need for long-term hemodialysis. However, more studies are needed to define the role of steroids and compare the benefits with the risks associated with such therapy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Glomerulonephritis associated with MRSA infection: A possible role of bacterial superantigen. Kidney Int. 1995;47:207-16.
- [Google Scholar]
- Post-MRSA infection glomerulonephritis with marked Staphylococcus aureus cell envelope antigen deposition in glomeruli. J Nephrol. 2006;19:215-9.
- [Google Scholar]
- A case of superantigen-related glomerulonephritis after methicillin-resistant Staphylococcus aureus (MRSA) infection. Clin Nephrol. 1997;48:311-6.
- [Google Scholar]
- IgA-dominant postinfectious glomerulonephritis: A report of 13 cases with common ultrastructural features. Human Pathology. 2008;39:1309-16.
- [Google Scholar]
- Staphylococcus infection-associated glomerulonephritis mimicking IgA nephropathy. Clin J Am Soc Nephrol. 2006;1:1179-86.
- [Google Scholar]
- Effective antibiotic treatment of methicillin-resistant Staphylococcus aureus-associated glomerulonephritis. Nephron. 2002;92:297-3.
- [Google Scholar]
- Glomerulonephritis causing acute renal failure during the course of bacterial infections.Histological varieties, potential pathogenetic pathways and treatment. Int Urol Nephrol. 2008;40:461-70.
- [Google Scholar]
- Successful treatment of post-MRSA infection glomerulonephritis with steroid therapy. Clin Nephrol. 2008;70:344-7.
- [Google Scholar]







