Translate this page into:
Pheochromocytoma of urinary bladder
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pheochromocytoma of urinary bladder are rare tumors. They present with nonspecific clinical signs and symptoms, so imaging plays an important role in diagnosing and localizing the tumor. We present two cases of bladder pheochromocytoma, one of them presented with vague abdominal pain and the other with hematuria. Biphasic CT in both the cases showed hypervascular intravesical mass suggestive of bladder pheochromocytoma. The lesions were confirmed biochemically or on postoperative histopathology. A brief review of the imaging in bladder pheochromocytoma is also presented.
Keywords
Pheochromocytoma
urinary bladder
hypertension
Introduction
Pheochromocytoma of urinary bladder accounts for less than 0.05% of all bladder tumors and less than 1% of all the pheochromocytomas.[12] Various imaging studies are helpful in the diagnosis and localization of the tumor. Metaiodobenzylguanidine (MIBG) scan is considered specific but has limited utility because of cost and restricted availability.[1] Pheochromocytomas are usually hypervascular, so biphasic CT play an important role in its diagnosis even in the patients where bladder phaeochromocytoma is not considered as clinical diagnosis.
Case Reports
Case 1
A 37-year-old female presented with vague abdominal discomfort for 2 years. On examination, she was found to be hypertensive. Hemogram, renal and liver function tests were normal. Ultrasound showed a lobulated 6.5×5 cm heterogeneously hyperechoic mass at right para-aortic region at level of renal hilum and a 3.5×2 cm lesion along posterior wall of the bladder. On biphasic CT [Figure 1], both the lesions showed hypervascularity. In addition, the bladder lesion showed small central speck of calcification. With the possibility of multifocal pheochromocytoma, MIBG scan was done which showed increased activity in the lesions. Patient underwent removal of the right para-aortic lesion and partial cystectomy. Pheochromocytoma was confirmed at both the sites on histopathology.
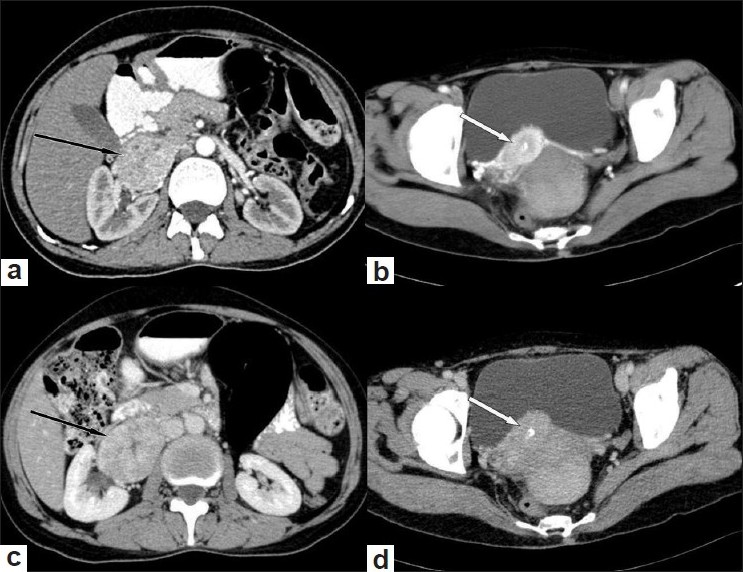
- Axial sections of CT in arterial (a,b) showing hyper enhancing lesions at right para-aortic region (black arrow) and along posterior wall of the urinary bladder (white arrow). These lesions showing relative contrast washout in venous phase (c,d). In addition, bladder lesion showed small central speck of calcification
Case 2
A 40-year-old male presented with recurrent and intermittent hematuria for last 2 years, and was recently detected to have hypertension. Ultrasound showed a 3×2 cm heterogeneous lesion at the bladder base with enlarged lymph nodes along right iliac vessels and perivesical region. Biphasic CT [Figure 2] showed hypervascular bladder lesion and lymph nodes. So possibility of malignant pheochromocytoma with lymph nodes metastases was kept. Basal urinary metanephrine excretion was extremely high, confirming the diagnosis. Patient underwent partial cystectomy with pelvic lymphadenectomy.
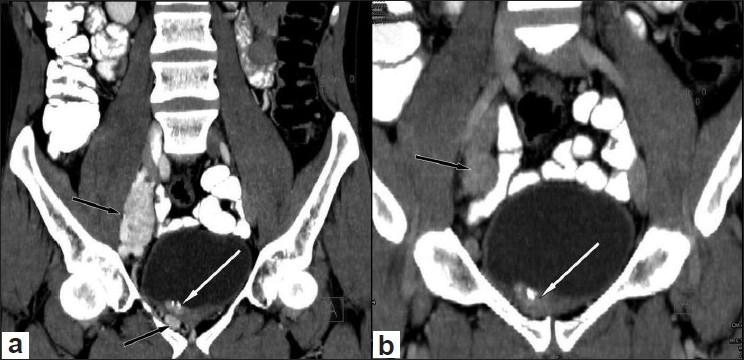
- Coronal reformatted CT images in arterial (a) and venous phase (b) depicting the bladder base lesion (white arrows) with enlarged lymph nodes along right iliac vessels and perivesical region (black arrow). The lesion and the lymph nodes are showing hypervascularity and there is coarse calcification in the bladder lesion
Discussion
Extra-adrenal pheochromocytoma (EAP) develops in the paraganglion chromaffin cells in the sympathetic nervous system and accounts for 10-15% of pheochromocytomas in the adults and 30-40% in children.[13] More than 85% of the tumors occur below the diaphragm with para-aortic region being the commonest site.[45] Other locations for the paragangliomas include gallbladder, urinary bladder, prostate, spermatic cord, uterus and duodenum.[4] EAP are usually sporadic. In adults these tumors are malignant in approximately 30-40% of patients compared to less than 2% in children. EAP tend to be larger than adrenal counterpart at the time of detection. Symptoms of EAP can be divided into two categories. The first category includes symptoms due to an excess of catecholamine and are similar to their adrenal counterpart. The second category includes symptoms that are due the specific location of the tumor and may help in its localization.
The bladder pheochromocytoma occurs between the third and fifth decade but may occur at any age.[3] They are usually submucosal or intramural with intact vesical epithelium, and are common in the region of the trigone.[4] The characteristic signs and symptoms of the bladder pheochromocytoma are hypertension and hematuria. Painless hematuria has been seen in 50-60% and hypertension in 65-80% patients.[4] These symptoms may be accompanied by headache, palpitations, hot flushes and sweating which may be aggravated by micturition or overdistension of the bladder. They are malignant in about 10% and may metastasize to regional lymph nodes or distant site. Imaging studies for the bladder pheochromocytoma include ultrasonography (USG), CT, MRI and MIBG.[56] On USG, they are seen as sharply circumscribed heterogeneously hypoechoic lesions. CT is widely available modality, providing high-resolution images in short time. Biphasic CT shows homogenous or heterogeneous hyperenhancing soft tissue masses.[6] Calcification may be seen in about 10% of the cases.[3] The tumors are usually hypointense to isointense on T1-weighted images, hyperintense on T2-weighted images and show avid contrast enhancement.[6] On cystoscopy, they appear granulated and lobulated, protruding into the bladder as globular yellowish, submucosal tumors. Irrigating the mass during cystoscopy can be helpful in confirm the diagnosis preoperatively as the blood pressure fluctuates. Cystoscopic biopsies are usually not advocated because positive rate is very low, bleeds easily and induces the blood pressure fluctuations.
Both the patients in our study were in the fourth decade with nonspecific clinical symptoms. Bladder lesions in both cases showed hypervascularity with coarse calcification. Case 1 was having extra-adrenal right para-aortic and bladder pheochromocytoma. Bladder lesions could have been missed if preoperative biphasic imaging had not been performed. In case 2, patient could have undergone transurethral resection (TUR) or other surgery without knowing its character leading to inadvertent complications. So in both our cases biphasic CT depicted hypervascular bladder lesion suggesting bladder pheochromocytoma. The preoperative diagnosis of the bladder pheochromocytoma is important because preoperative preparation (requires the similar preoperative stabilization of hypertension strategy as other pheochromocytomas) and intraoperative (cystoscopic examination prior to the excision to delineate the exact location of the lesion, depth of invasion and the involvement of the ureters) treatment varies as compared to the other bladder lesions. In addition, the preferred treatment to the bladder pheochromocytoma is open surgery rather than TUR of bladder tumors or laparoscopic partial cystectomy.
To conclude, pheochromocytoma (paragangliomas) should always be considered as in the differential diagnosis of hypervascular lesions in the bladder. Transitional cell carcinoma of the bladder is a hypovascular lesion. Patients having atypical morphology bladder lesion, abdominal paragangliomas and varied symptoms associated with micturition should undergo biphasic CT. It may help in the diagnosis of bladder pheochromocytoma, even if there is no characteristic clinical history or clinical suspicion, by showing its hypervascularity.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Pheochromocytoma of the urinary bladder without typical symptoms. Int J Urol. 2003;10:398-400.
- [Google Scholar]
- Malignant paraganglioma of the urinary bladder: A case report. Int Urol Nephrol. 2001;33:343-5.
- [Google Scholar]







