Translate this page into:
Posterior reversible encephalopathy syndrome in minimal change disease
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
An 11-year-old girl was being treated elsewhere from the age of 5 years for nephrotic syndrome. She received prednisolone 30 mg per day until remission followed by tapering. She had several relapses during the last 5 years, and presented to us in nephrotic state. Her pulse rate and blood pressure were 78 bpm and 90/70 mmHg, respectively. Systemic examination was unremarkable. Investigations revealed blood urea: 12 mg/dL, serum creatinine: 0.7 mg/dL, serum proteins: 4.7 g/dL, serum albumin: 2.1 g/dL, 24 h urine protein: 4.5 g, serum cholesterol: 450 mg/dL, serum LDL: 267 mg/dL, serum HDL 60 mg/dL, serum VLDL: 158 mg/dL, serum triglycerides 615 mg/dL, hemoglobin: 12 g/dL. Renal biopsy revealed 11 glomeruli, and findings were consistent with minimal change. She received 65 mg of prednisolone in three divided doses per day according to the ISKDC protocol.[1] After 3 weeks, she presented with multiple episodes of generalized tonic clonic seizures. She was afebrile, pulse rate was 160 bpm, blood pressure was 110/60 mmHg. Glasgow coma scale was 7/15. Cerebrospinal fluid analysis revealed 3 cells/hpf, glucose: 56 mg/dL, protein: 15 mg/dL. MRI brain showed bilateral asymmetrical T2, FLAIR hyperintense lesions in cortical and subcortical location of parieto-occipital, temporal lobes, bilateral thalami, and cerebellum suggestive of posterior reversible encephalopathy syndrome (PRES)[Figure 1]. She was treated with antiepileptics and the dose of prednisolone was reduced to half. She recovered completely in 48 h.
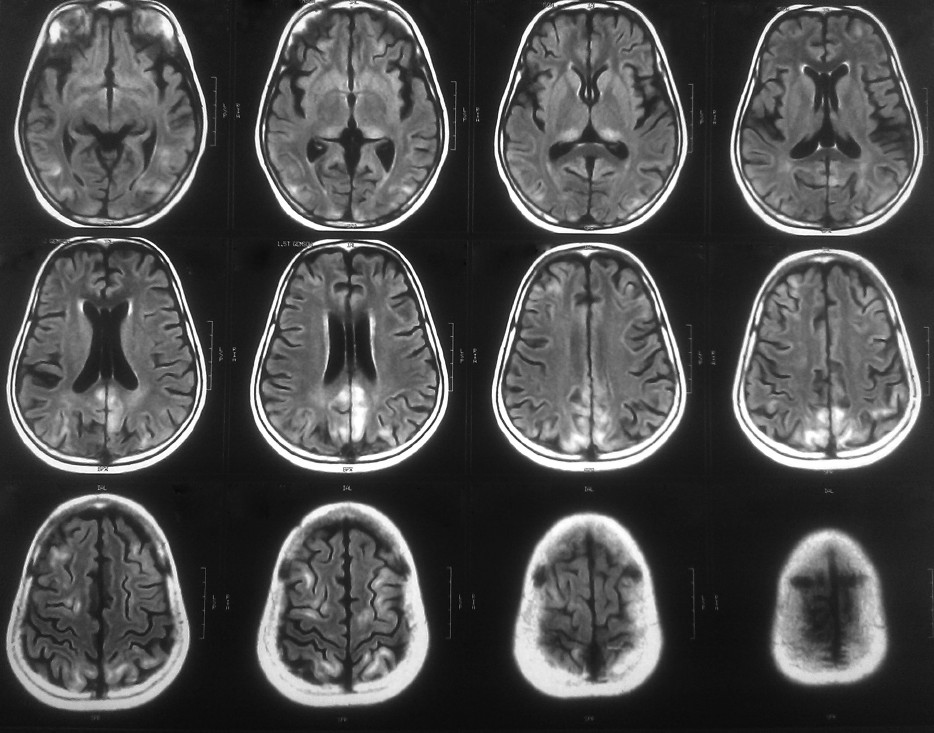
- MRI brain: Posterior reversible encephalopthy syndrome
PRES, originally termed reversible posterior leukoencephalopathy syndrome[2] presents with headache, seizures, visual changes, altered mental status, and occasionally focal neurologic signs.[3] CT and MR imaging typically show symmetrically distributed areas of vasogenic oedema predominantly within the territories of the posterior circulation.[3]
PRES is seen with a heterogeneous group of disorders.[3] In renal disorders, it is reported with hemolytic the uremic syndrome, thrombotic thrombocytopenic purpura, as a complication of Cyclosporine and tacrolimus,[34] and acute poststreptococcal nephritis[4] In patients with the nephrotic syndrome, the risk factors are administrationof cyclosporine, tacrolimus,[4] methylprednisolone,[5] hypertension and renal insufficiency.
However, nephrotic syndrome itself could be considered a predisposing condition for developing PRES in both adults and children.[6] The key pathophysiological process of PRES is vasogenic edema.[2] due to decreased intravascular oncotic pressure, increased permeability of intracerebral capillaries, and fluid overload. Drugs such as cyclosporine, tacrolimus, and methylprednisolone may induce vasogenic oedema by alterating sympathetic flow, cyclosporine-mediated release of endothelin, or endothelial dysfunction, while hypertension may also induce oedema due to autoregulation failure of the cerebral blood flow.
References
- Report of International Study of Kidney Disease in Children: The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr. 1981;98:561-4.
- [Google Scholar]
- A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494-500.
- [Google Scholar]
- Posterior reversible encephalopathy syndrome: Prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002;23:1038-48.
- [Google Scholar]
- Posterior reversible encephalopathy syndrome in children: Its high prevalence and more extensive imaging findings. Am J Kidney Dis. 2006;48:231-8.
- [Google Scholar]
- Reversible posterior leukoencephalopathy in a patient with minimal-change nephrotic syndrome. Am J Kidney Dis. 2001;37:E30.
- [Google Scholar]
- Hypertensive encephalopathy and nephrotic syndrome: A possible link? Nephrol Dial Transplant. 1999;14:1750-2.
- [Google Scholar]






