Translate this page into:
Acute interstitial nephritis and drug rash with secondary to Linezolid
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Linezolid, a member of oxazolidinone antibiotic class, is a relatively well-tolerated drug with few side effects. It is active against gram-positive cocci, including multidrug resistant staphylococci and enterococci. We report a case of a 54-year-old diabetic male with alcoholic cirrhosis admitted in intensive care unit with altered sensorium. He was diagnosed as a case of hepatic failure secondary to hepatitis E infection and enterococcal urosepsis. He was started on linezolid based on the urine culture sensitivity report. On day three of linezolid treatment, he developed severe pruritus, macular rash, eosinophilia, and renal dysfunction. Renal biopsy showed acute tubulointerstitial nephritis. Renal functions improved on discontinuation of linezolid and short course of steroid therapy.
Keywords
Acute interstitial nephritis
drug rash with eosinophilia and systemic symptoms syndrome
linezolid
Introduction
Acute interstitial nephritis (AIN) defines a pattern of renal injury usually associated with an abrupt deterioration in the renal function characterized histopathologically by inflammation and edema of the renal interstitium.[1] AIN is an important cause of acute kidney injury caused by drug hypersensitivity reactions, especially in intensive care units, where patients are usually receiving multiple drugs including antibiotics. Penicillin and cephalosporin are the leading causes of drug-induced AIN. Recently, linezolid, a member of oxazolidinone antibiotic class, has been found to be associated with AIN and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome.
Case Report
A 54-year-old male case of alcoholic cirrhosis (Child A) and diabetes mellitus without any evidence of nephropathy was admitted at our center with 2-day history of altered sensorium and fever. There was no prior history of headache, vomiting, seizures, or decreasing urine output. On physical examination, patient was febrile, disoriented, pulse rate was 100/min, blood pressure was 150/70 mmHg, mild icterus, and pedal edema was present. There was no evidence of focal neurological deficit or signs of meningism. Fundus examination revealed no features of papilledema or retinitis. Bilateral pupils were equal and reacting to light. Abdominal examination revealed free fluid with no organomegaly whereas other systems were unremarkable.
Lab investigations revealed Hb 9.6 gm/dL, total leukocyte count (TLC) 16 800/ mm3 with normal eosinophil counts and platelet count 1.1lac/mm3, with normal coagulation profile with INR of 1.3. Serum bilirubin was 3.0 mg/dL with AST/ALT of 87/96 IU/L. Arterial ammonia was 239 μg/dL. Viral markers were positive for IgM anti-HEV; however, HBsAg, anti-HCV, IgM anti-HAV, and HIV were negative. Ascitic fluid analysis revealed high ascites with high serum-ascites albumin gradient normal cell counts. His ultrasonography abdomen was suggestive of chronic liver disease with coarse echotexture and normal bilateral kidneys. Renal functions were normal with 1+ proteinuria with full field leucocytes and 8-10 RBC/high-power field on urine analysis. Urine culture was positive for enterococcus faecalis, with sensitivity to linezolid only.
Patient remained in altered sensorium, and was diagnosed as a case of hepatic encephalopathy and uro-sepsis on the basis of positive urine culture. He was managed with lactulose and supportive care for liver failure. Linezolid 600 mg twice a day was started in view of positive urine culture for enterococcus. On day 3 of linezolid therapy, he developed pruritus, erythematous macular rash involving all the extremities and trunk. Peripheral blood smear showed eosinophilia with an absolute eosinophil count of 2125 cells/mm3. His serum IgE levels were also elevated (430 IU/mL). Repeat urine examination revealed 2+ proteinuria with 15-20 leukocytes with WBC casts and RBC cast, with no evidence of eosinophils. Renal functions were deranged with serum creatinine rising upto 5.2 mg/dL with decreasing urine output requiring dialytic support. Dermatological opinion was taken and a diagnosis of DRESS syndrome was made. Keeping the clinical possibility of drug-induced AIN as a cause of renal dysfunction, his drugs were reviewed and linezolid was stopped. The rash and fever subsided in a few days. However, the renal functions remained deranged. Patient recovered from hepatic encephalopathy and liver functions showed improvement. Further investigations revealed ANA and ANCA to be negative, with normal complement levels.
Renal biopsy was performed in view of persistently deranged renal functions and microscopic hematuria. H-stained section showed normal glomeruli on light microscopy. Interstitium showed edema with moderate inflammatory infiltrate comprising predominantly of mononuclear cells with few eosinophil and proximal tubular dilatation with patchy necrosis [Figure 1]. Birefringent oxalate crystals were also present in tubules and interstitium with foreign body giant cell reaction [Figure 2]. There was no granuloma formation. The arterioles were unremarkable, with no evidence of vasculitis or thrombosis. Immunofluoroscence examination of biopsy showed no immune complex deposition. Thus, the renal biopsy established the diagnosis of acute tubulointerstitial nephritis with patchy tubular necrosis.
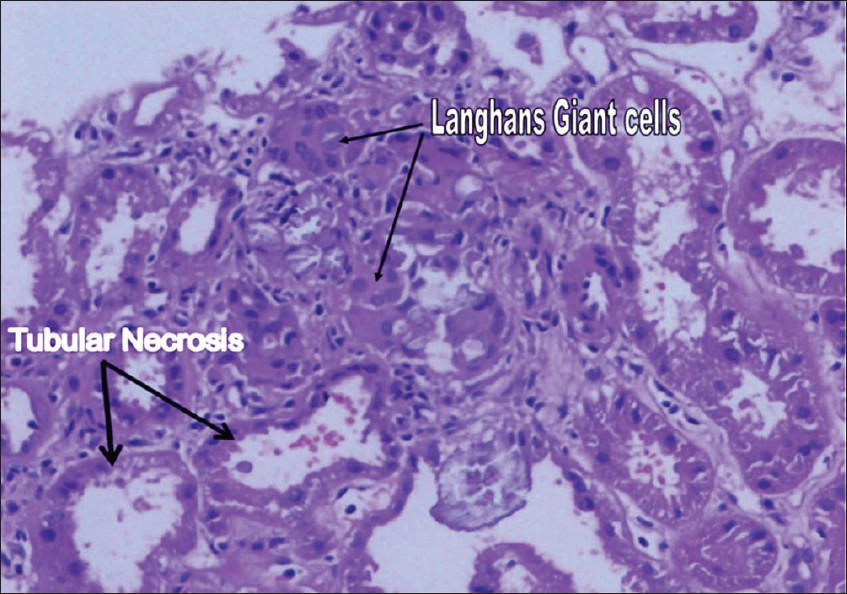
- Patchy tubular necrosis and foreign body giant cell reaction to oxalate crystals in the interstitium

- Oxalate crystals in tubules and mononuclear cell infiltrate in the interstitium
Patient was managed with short course of prednisolone for 2 weeks. Renal functions gradually improved with serum creatinine level decreasing to 1.4 mg/dL, which corresponds to an estimated creatinine clearance of 56 mL/min. Patient is being regularly followed-up and has not shown any deterioration in renal functions.
Discussion
AIN is a common cause of acute kidney injury. The incidence of AIN in patients biopsied for acute renal failure has been reported to be approximately 5-15%.[2] The common underlying etiologies include drug-induced, infection-related, autoimmune, and idiopathic forms. The most common etiology of AIN is drug-induced disease, which is thought to underlie 60-70% of cases. Backer et al. reviewed about 128 patients of AIN and found drugs to be responsible for 71% cases with antibiotics responsible for around 1/3 of all.[3]
Linezolid, potent antibiotic with excellent activity against multidrug-resistant gram-positive bacteria and good safety profile, has recently been found to be associated with DRESS syndrome and AIN presenting as acute kidney injury.[4–6] Our patient developed nonoliguric renal failure, macular rash, pruritus, and eosinophilia 3 days after linezolid exposure. All other drugs known to cause AIN were excluded one by one; however, renal dysfunction improved only after withdrawal of linezolid and corticosteroid therapy. This is a strong supporting evidence of linezolid associated DRESS syndrome with accompanying AIN confirmed on renal biopsy.
The DRESS syndrome is a hypersensitivity reaction, characterized by a widespread and long-lasting papulopustular or erythematous skin eruption often progressing to exfoliative dermatitis with fever, lymphadenopathy, and visceral involvement (hepatitis, pneumonitis, myocarditis, pericarditis, and nephritis) and accompanied by blood alterations like eosinophilia in about 90% and mononucleosis in about 40% of cases.[78] Anticonvulsants, sulfonamides, dapsone, allopurinol, minocycline, and gold salts are among the most frequent culprit drugs.
Linezolid-associated AIN with or without DRESS syndrome has been described in only three patients till now. Report by Savard et al. described an 88-year-old patient developing DRESS syndrome with AIN and mild hepatitis following linezolid, almost 7 days after initiation of therapy. As in our case, the renal biopsy of this patient also showed deposition of oxalate crystals, without any evidence of secondary hyperoxaluria. In another report, Hammer et al. reported linezolid-induced AIN in a patient with tibial osteomyelitis. Withdrawal of linezolid, short-term hemodialysis, and corticosteroid therapy led to resolution of symptoms and eventual recovery of the renal function. Residual renal insufficiency was not a feature of AIN in these patients with native kidneys in contrast to our case. Esposito et al. reported a renal transplant patient developing AIN without systemic symptoms on exposure to linezolid for management of an enterococcus faecium abscess of a huge liver cyst.
Renal biopsy is the only definitive method of establishing the diagnosis of AIN. Biopsy is usually done when either the diagnosis is not clear or patient does not show improvement in the renal function, despite discontinuation of suspected drug. Adverse prognostic factors in AIN recovery include diffuse versus patchy inflammation on biopsy, excess number of neutrophils (1% to 6%) and extent or severity of interstitial fibrosis, which correlates with the final glomerular filtration rate.[9] Noninvasive tests such as ultrasonography, gallium scintigraphy, and eosinophiluria have limited diagnostic utility.
The mainstay of therapy for drug-induced AIN is early discontinuation of the suspected drug. There are no randomized trials to support the use of corticosteroids in treatment of AIN; however, the decision to use steroids depends upon the clinical course following withdrawal of offending drug. In general, the prognosis for drug-induced AIN is good, and at least partial recovery of the kidney function is normally observed. Early recognition is crucial because patients can ultimately develop chronic kidney disease.
In conclusion, AIN and DRESS syndrome are rare adverse effects of linezolid. Early detection of this rare adverse reaction and prompt discontinuation of the offending agent may potentially prevent acute kidney injury. This case indicates that linezolid can cause AIN, and we recommend close monitoring of renal function in patients who are prescribed this drug.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Diagnosis and management of acute interstitial nephritis. Am Fam Physician. 2003;67:2527-34.
- [Google Scholar]
- The changing profile of acute tubulointerstitial nephritis. Nephrol Dial Transplant. 2004;19:8-11.
- [Google Scholar]
- Linezolid-induced interstitial nephritis in a kidney-transplant patient. Clin Nephrol. 2007;68:327-9.
- [Google Scholar]
- Linezolid-associated acute interstitial nephritis and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Am J Kidney Dis. 2009;54:e17-20.
- [Google Scholar]
- The drug hypersensitivity syndrome: What is the pathogenesis? Arch Dermatol. 2001;137:357-64.
- [Google Scholar]
- Drug-induced pseudolymphoma and hypersensitivity syndrome.Two different clinical entities. Arch Dermatol. 1996;132:1315-21.
- [Google Scholar]
- Prediction of the long-term outcome in acute interstitial nephritis. Clin Nephrol. 1984;22:55-60.
- [Google Scholar]







