Translate this page into:
Spectrum of renal lesions in systemic lupus erythematosus: Six years’ experience at a tertiary health care centre in north east India
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
SLE has an incidence of 3-4 in 100,000 populations per year in India.[1] Its clinical features show regional variations.[2] Renal involvement is seen in 1/3rd of patients.[3] However, there are no data on SLE in the north-eastern part of the country. We hereby present the spectrum of renal lesions encountered in SLE patients in our Institute.
A total of 30 patients with SLE and clinical renal disease were diagnosed between 2006-2011. Out of these, three cases were known cases on treatment and 27 cases came to the hospital for the first time. Two cores of renal biopsies taken under ultrasound guidance, after an informed consent, were processed routinely and stained using haematoxylin and eosin stain, Periodic acid Schiffs stain, Gomoris methenamine silver stain and Masson trichrome stain. Immunohistochemical evaluation using IgG, IgA, IgM, C3 and C1q antibodies was done when tissue was adequate.
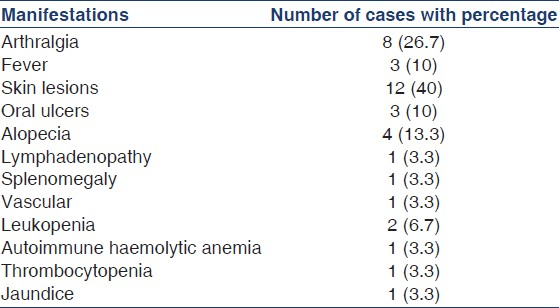
Most patients were in the age group of 21 to 30 years with a median age of 24 years. There were 28 female and two male patients. The youngest patient was a 13 year-old female. Renal manifestations ranged from decreased renal output to hematuria and nephrotic syndrome. Most of the patients had puffiness of face, bilateral pedal oedema, ascites and pleural effusion [Table 1]. The haemoglobin ranged from 7 to 10.4 gm/dl. Serum creatinine was raised in four patients (1.4-2.4 mg/dl). Proteinuria ranged from 2 + to 3 + with 24 hrs urine protein level of 1.8 to 3 gm. There was hypoalbuminemia of < 1.5 gm/dl in 20 patients.
Majority of the cases had class IV disease (n = 16), followed by class III (n = 6), II (n = 5) and V (n = 3) as per the revised ISNRTP criteria. As facility for immunofluorescence was not available during the study period, 15 cases with adequate tissue were also subjected to immunohistochemistry using IgG, IgA, IgM, C3 and C1q antibodies. The class II lupus nephritis showed mesangial deposits of IgG, C3, IgA and IgM and class III, class IV and V lupus nephritis showed full house pattern with mesangial and endocapillary deposits which correlated with the degree of light microscopic changes. Electron microscopy could not be done because of lack of facilities.
In India, lupus nephritis occurs in about half of SLE patients ranging from 35-70% taking the criteria for diagnosis of lupus nephritis as proteinuria of + + + or > 0.5 gms/24 hr.[2] Lupus nephritis was diagnosed at the time of first hospital admission in 90% of our patients in conformity with the studies by Niang et al. and Ballow et al.[45] Our study showed nephrotic range proteinuria in 66.6% of cases. Studies have shown nephrotic range proteinuria ranging from 20 to 50%.[46]
Our study showed a predominance of Class IV lesions. This finding has been previously reported in many other series.[78] All the class II cases had clinical evidence of renal disease ranging from nephritic to nephrotic syndrome. The renal biopsy findings correlated with the degree of renal manifestations and helped the clinician in deciding the protocol of treatment. Short term prognosis was good in our patients. But, most of the cases were lost to follow up and no follow up biopsies could be taken for comparison except in one case of class II lupus nephritis that came with recurrence of symptoms and showed class V lupus nephritis with active lesions on repeat biopsy.
In conclusion, this study revealed that the chances of lupus nephritis presenting with nephrotic syndrome is higher in this region. Absence of facilities for Immunofluorescence and electron microscopy in a resource poor area like ours should not be a hindrance to provide adequate information based on light microscopy, as these facilities would have only added additional information in cases of lupus nephritis. Due to unawareness, our patients seek medical help only after they develop overt manifestations of renal disease, which is a matter of concern and need to be addressed.
References
- Retrospective analysis of patients with lupus nephritis: Data from a large clinical immunological centre in Hungary. Scan J Immunol. 2006;64:43-7.
- [Google Scholar]
- Lupus nephritis in Senegal: A study of 42 cases. Saudi J Kidney Dis Transpl. 2008;19:470-4.
- [Google Scholar]
- Lupus nephropathy in internal medicine.About 44 cases. Rev Med Interne. 2003;24(S4):433-4.
- [Google Scholar]
- Immuno-histologic changes in lupus nephritis in female patients. A four year study. Saudi J Kidney Dis Transpl. 2008;19:658-63.
- [Google Scholar]
- Lupus nephritis in an AfroCaribbean population: Renal indices and clinical outcomes. Lupus. 2006;15:689-94.
- [Google Scholar]






