Translate this page into:
Sternal tuberculosis in a patient with chronic kidney disease
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Sternum is generally regarded as resistant to infections and thus is an infrequent site of osteomyelitis. Involvement of sternum by Mycobacterium tuberculosis is rare. Sternal tuberculosis in chronic kidney disease (CKD) was not reported till date. We report a 40-year-old patient with stage IV CKD, who presented with sternal and cervical lymphnodal tuberculosis.
Keywords
Chronic kidney disease
sternum
tuberculosis
Introduction
Sternal tuberculosis is uncommon both in the developing and developed countries.[1] Till 2009, only 25 cases had been reported in peer-reviewed journals.[2] The diagnosis is delayed because of the rarity, nonspecific symptoms, slowly progressive course, and paucibacillary state. The incidence of tuberculosis in chronic kidney disease (CKD) was reported to be around 4%, with extrapulmonary forms of tuberculosis dominating the pulmonary forms.[3] We describe a patient with stage IV CKD with tuberculosis of sternum and cervical lymphnodes. To our knowledge, this may be the first case of sternal tuberculosis in CKD.
Case Report
A 40-year-old man with CKD presented with painless, slowly growing swelling over the lower part of the sternum of 20 days′ duration. There was no history of trauma or local surgery preceding its appearance. He had received treatment for pulmonary tuberculosis 11 years ago and for lymphnode tuberculosis 8 years ago. There was a history of loss of weight of 5 kg over 2 months prior to presentation. There was no history of fever and night sweats. On examination, he was malnourished with right-sided cervical lymphadenitis with matting. There was a 4 cm × 3 cm fluctuant painless swelling in the lower 1/3rd of sternum with no discharge or sinus formation [Figure 1]. Evaluation revealed anemia with hemoglobin 8.8 gm/dl, normal total leukocyte count 4900 /mm3, elevated erythrocyte sedimentation rate 120 mm blood urea 85 mg/dl and serum creatinine 3.26 mg/dl, and serum albumin of 3.1 gm/dl. Chest radiograph revealed old fibrotic strands in the lung parenchyma suggestive of pleuropulmonary tuberculosis. Computer tomography of the chest showed destruction of lower part of the sternum with adjacent abscess formation [Figure 2]. Fibrotic strands were present in the left upper lobe and apical segment of the left lower lobe. Tuberculin skin test was negative. Fine needle aspiration cytology of the sternal swelling was carried out and it revealed areas of necrosis with epithelioid giant cells in clusters. Polymerase chain reaction (PCR) for tuberculous bacillus was positive. Excision biopsy of right cervical lymph nodes revealed numerous epithelioid granulomas with central caseation and surrounded by Langhans giant cells. Keeping the diagnosis of sternal and lymphnodal tuberculosis in view, he was started on antituberculosis therapy. With the four-drug antituberculosis therapy, the patient showed significant improvement. The sternal lesion and the cold abscess resolved.

- Clinical picture showing a swelling in the lower 1/3rd of sternum around 4 cm × 3 cm in size
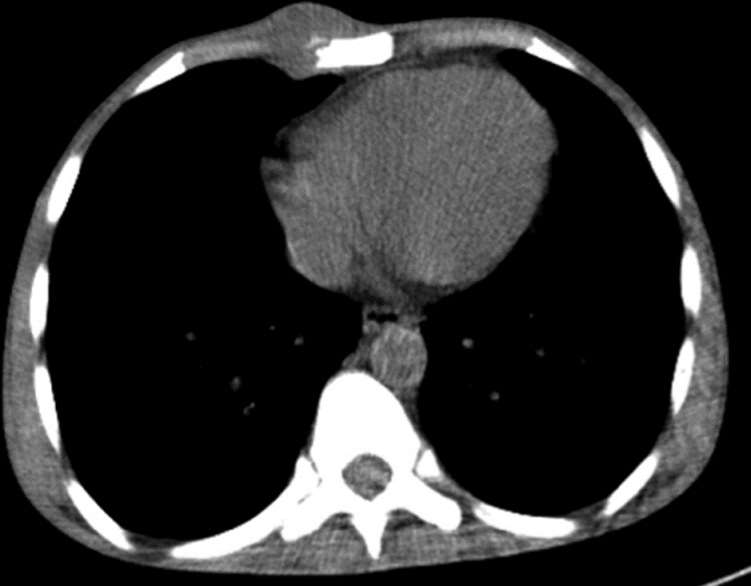
- Computed tomography of the chest showing destruction of the lower part of the sternum along with adjacent soft tissue mass and abscess formation
Discussion
Tuberculosis continues to be a major global problem, particularly in the developing countries. The incidence of Skeletal tuberculosis was reported to be 6-10% of extrapulmonary TB,[34] and this is due to the impaired cellular immunity and malnutrition. Sternal involvement in tuberculosis can occur as an isolated involvement or due to spread from a focus elsewhere in the body. The spread is by hematogenous or lymphatic route, or due to contiguous spread. The clinical presentation of the external tuberculosis is variable, often presenting as a painful slowly progressive swelling with an insidious course. Sternal radiographs are often nonspecific and may not provide clues to the diagnosis. Computed tomography has traditionally been used for evaluation of tuberculous involvement of sternum and is helpful as it also picks up pleuropulmonary lesions. Magnetic resonance imaging is now being used increasingly as it picks up additional soft tissue changes.[5]
Fine needle aspiration cytology is the most commonly used technique for establishing the diagnosis as it is easy and inexpensive. The material obtained from aspiration/biopsy can be studied by Ziehl-Neelsen staining for acid-fast bacillus, culture on Lowenstein-Jensen media, deoxyribonucleic acid (DNA) detection by PCR, and histopathology.[2] About 1% of skeletal tuberculosis affects the sternum.[1] Patients with CKD who are found to have sternal tuberculosis are treated with isoniazid, rifampicin, ethambutol, and pyrazinamide for two months in the initial phase, followed by a 6-12-month regimen of maintenance phase with isoniazid and rifampicin. Surgical treatment is decided based on the extent of bony destruction, associated complications, and response to therapy.
In our patient, the diagnosis of sternal tuberculosis was established based on radiological, microbiological, and histopathological features. Computed tomography of the sternum revealed destruction of the lower part of the sternum with adjacent abscess and fibrotic strands in the left upper lobe and apical segment of left lower lobe. Furthermore, the fine needle aspiration findings favored tuberculosis and the material aspirated from the swelling was positive for Mycobacterium tuberculosis on PCR. In addition, histopathology of the lymphnodal mass was suggestive of tuberculosis.
We suppose the sternal tuberculosis in our patient was due to reactivation of the latent bacilli as he had a history of pleuropulmonary tuberculosis. His immunocompromised and malnourished state due to CKD would have made him susceptible to reactivation, thus leading to sternal and lymphnodal tuberculosis. In conclusion, our presentation highlights the occurrence of a rare entity of sternal tuberculosis in a patient with CKD, and its favorable response to therapy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Spontaneous fracture of the sternum and sternal tuberculosis. Thorax. 1987;42:984-5.
- [Google Scholar]
- Primary Sternal tuberculous osteomyelitis: A case report and discussion. Can J Infect Dis Med Microbiol. 2009;20:e181-4.
- [Google Scholar]
- Tuberculosis of sternum: three cases with different presentations. J Assoc Physicians India. 2009;57:595-6.
- [Google Scholar]







