Translate this page into:
Anesthetic management in parturients with chronic kidney disease undergoing elective Caesarean delivery: Our experience of nine cases
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
In this retrospective study, we describe the anesthetic management and its implications in parturients with chronic kidney disease (CKD; n = 9), who underwent elective caesarean delivery. Nine parturients with CKD of various etiologies, who underwent elective Caesarean delivery, were included in this study. Spinal anest-hesia was administered in all parturients with normal coagulation profile through a 25-gauze spinal needle (Quincke) with 0.5% (H) bupivacaine in L2-3 space and T6 level was achieved. Hemodynamics and side effects such as nausea, vomiting, headache, and backache were record. The mean age was 28.22 ± 4.43 years. The mean levels of serum creatinine and serum potassium were 2.78 ± 1.29 mg/dl and 4.11 ± 0.46 meq/l, respectively. Mean baseline values of systolic blood pressure, diastolic blood pressure, and pulse rate were higher which decreased after spinal anesthesia. However, the incidence of hypotension, which required mephentermine treatment, was 11.1%. One patient had symptoms of nausea and vomiting/dizziness at the time of hypotension, which disappeared after treatment with 5 mg of intravenous mephentermine. Baseline value of PR remained high throughout the operation. Parturients with CKD with normal coagulation profile remained hemodynamically stable under spinal anesthesia with minimal side effects. However, a large number of studies are required to determine the safety of spinal anesthesia in this setting.
Keywords
Caesarean delivery
chronic kidney disease
pregnancy
spinal anesthesia
Introduction
Renal disease during pregnancy is relatively uncommon. Several factors must be considered when managing pregnant women with chronic kidney disease (CKD) to minimize the adverse effects of pregnancy and kidney disease on mother and consequent effects on the fetus. The kidneys undergo pronounced hemodynamic, renal tubular, and endocrine changes during pregnancy. During healthy pregnancy, kidney increases the production of erythropoietin, active vitamin D, and renin. Patients with CKD are prone to disturbances of electrolytes, acid-base, and fluid homeostasis. Anesthesia for such patients entails many risks such as cardiovascular instability, alteration of drug metabolism, increased gastric acid secretion, and platelet dysfunction. There is paucity of information regarding the safe conduct of anesthesia in this group of patients. Spinal anesthesia is a safe and preferred technique for Caesarean delivery of normal parturient. Here, we have discussed anesthetic management and its implications in parturients with CKD on medical management/required dialysis during pregnancy who underwent elective Caesarean delivery.
Materials and Methods
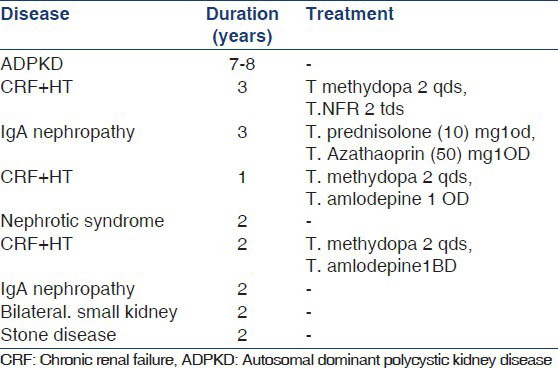
This retrospective study was designed after obtaining approval from the institutional ethics committee, and nine parturients with CKD aged 22-34 years who underwent elective Caesarean delivery for obstetrical indications between January 2010 and March 2011 were analyzed. Table 1 shows their disease, duration, and treatment of illness. Two patients required hemodialysis in third trimester. Table 2 shows investigations. Pre-operative hemodialysis, morning dose of treatment drug, serum potassium and coagulation profile were advised. Acid prophylaxis was given in the form of ection Ranitidine and Injection ondansetrone. In the operation theater, intravenous access was established with 18G cannula. Intraoperatively, patients were monitored with, Electrocardiogram, Noninvasive blood pressure and SpO2. All patients received 0.9% normal saline. Spinal anesthesia was administered through a 25-gauze spinal needle with Inj. bupivacaine (0.5%) in L3-4 space and T6 level was achieved. After delivery of baby and placenta, Inj. prostodin intramuscularly and intravenous Inj. oxytocin were given. Injection tramadol 2 mg/kg was given intravenously for post-operative analgesia. After completion of surgery, patients were shifted to ICU and observed for nausea, vomiting, headache, and backache.

Statistical analysis
Statistical analysis was performed using SPSS version 12. Data were expressed as mean ± SD.
Results
Demographic data [Table 3], spinal puncture to skin incision, skin incision to skin closure, and uterine incision to delivery intervals, and 5-min Apgar scores [Table 4], and etiology of their disease were shown in Table 1.


The mean value of Hb was 10.1 ± 0.78 g/dl%. Three patients were on antihypertensive therapy: Methyldopa and nifedepine tablets. BP and PR values were shown in Figures 1-3. Mean baseline values of SBP and DBP were higher which decreased after spinal anesthesia However, the magnitude of decrease in BP was small. The incidence of hypotension, which required mephentermine treatment, was 11.1%. One patient had symptoms of nausea, vomiting, or dizziness at the time of hypotension, which disappeared after treatment with 5 mg of injection mephentermine. Baseline value of PR remained high throughout the operation. The mean values of serum creatinine and serum potassium K+ were 2.78 ± 1.29 mg% and 4.11 ± 0.46 meq/l, respectively. None of our patients had backache or headache.

- Mean pulse rate after spinal anesthesia

- Mean systolic blood pressures after spinal anesthesia

- Mean diastolic pressures after spinal anesthesia
Discussion
CKD is defined as either a Glomerular Filtration Rate <60 ml/min 1.73 m2 for 3 months or more or kidney damage leading to a decrease in GFR for 3 months or more. The damage may manifest as abnormalities in the composition of blood or urine, or radiological imaging or in histology. It is classified into five stages depending on GFR.[1]
The kidneys undergo pronounced hemodynamic, renal tubular, and endocrine changes during pregnancy. During healthy pregnancy, kidney increases the production of erythropoietin, active vitamin D, and renin. Women with CKD are less able to make the renal adaptations needed for a healthy pregnancy. Their inability to boost renal hormones often leads to normochromic normocytic anemia, reduced expansion of plasma volume, and vitamin D deficiency and the gestational rise in GFR is blunted.[2] The choice of anesthesia depends on the individual basis; however, regional anesthesia is preferred to minimize the risk of fetal depression and aspiration pneumonitis in the mother. While giving general anesthesia in patients with CKD, the effects of an altered clearance, the production and accumulation of active metabolites, and the risk of aggravating pre-existing kidney disease on drug administration must be considered. CKD may influence both the pharmacokinetics and the pharmacodynamics of a drug. Drug absorption may be altered by: Gastroparesis causing delayed gastric emptying, raised gastric PH caused by gastric urease, converting urea to ammonia, and gut edema. Reduced intestinal P-glycoprotein transporter found on the apical cell surface of small and large intestine mucosal cells which protects the body against toxic compounds by transforming them into the intestinal lumen activity in CKD may lead to increased intestinal absorption and bioavailability of certain compounds.[3] There is increased risk of aspiration pneumonitis under general anesthesia because of decreased gastric motility and prolongation of gastric emptying time. Hyperkalemia is a major concern while selecting the drug. Hyperkalemia is often induced by insufficient hemodialysis before surgery, acidosis, hypercapnia, hypoxemia, decreased body temperature, blood transfusion, and administration of suxamethonium.[4] Suxamethonium is known to induce 0.5-0.7 meq/l increase in serum K+ in the patients with chronic renal failure.[5] Anesthetic agents are transferred to the fetal especially barbiturates[56] resulting in sleeping baby which is detrimental to babies of CKD mothers. Metabolism of methoxyflurane and sevoflurane results in elevated fluoride levels which can cause further renal damage.[7]
CKD is associated with anemia, altered coagulation, metabolic acidosis, delayed gastric emptying, volume overload, and hyperkalemia.[8] Therefore, the safe conduct of anesthesia is mandatory for these patients. Pre-operative evaluation of the patient with CKD should focus on the comorbidities associated with kidney disease and on the signs and symptoms of uremia, fluid overload, and inadequate dialysis. Laboratory studies should include serum creatinine, electrolytes, Hb, platelet count, coagulation profile, and acid-base status.
Anemia is common in patients with CKD, so curing of anemia is important because this is a cause of left ventricular hypertrophy, heart failure, and angina. Curing of anemia also helps to improve the platelet dysfunction associated with CKD. In our study, CKD parturients were anemic and two patients required packed cell volume transfusion during dialysis. On the day of surgery morning, S. K and an ECG were obtained to screen for changes caused by electrolyte abnormalities especially hyperkalemia.[9] Electrolytes should not be measured immediately after dialysis due to incomplete equilibration between plasma and intracellular fluids. We observed normal serum potassium in all patients. Another feature of CKD is platelet dysfunction which is not related to a low platelet count. Patients who are receiving adequate dialysis are less likely to have significant platelet dysfunction and their risk of bleeding is less.[5] Platelet counts were normal in all our patients and none of them required platelet-rich plasma. Dialysis-dependent patient should receive dialysis before the operation to achieve a volume status as close to normovolemic as possible and to allow the patient to tolerate fluid loads required during surgery and also to obtain normal electrolyte concentration. Two of our patients received pre-operative dialysis.
The dosage of local anesthetic agents which are used for spinal anesthesia has been reported to exert no influence upon the baby.[5] In contrast to spinal anesthesia, epidural anesthesia requires large amounts of local anesthetic and the Intrauterine growth retardation fetus and neonate may be affected adversely by placental transfer of these drugs.[7] However, 50-60% of cases of spinal anesthesia experience hypotension followed by decreased uterine blood flow. In our study, we observed stable hemodynamics. For post-operative analgesia, fentanyl, sufentanil, and morphine can be added with local anesthetic in spinal anesthesia but we have avoided these opioids because our patients had IUGR babies.
The limitations of our study are: Our sample size is very small; and as it is a retrospective study, we need large number of patients. But unfortunately, few patients reach till full term of pregnancy. Based on our results, we consider that spinal anesthesia is safe to the patients with CKD if there is no platelet dysfunction or coagulation abnormalities.[1011]
Conclusion
This study showed that parturients with CKD with normal coagulation profile remained hemodynamically stable under spinal anesthesia with minimal side effects. However, a large number of studies are required to determine the safety of spinal anesthesia in this setting.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Recent developments in the perioperative management of adult patients with chronic kidney disease. Br J Anaesth. 2008;101:296-310.
- [Google Scholar]
- Renal disorders. In: James DK, Steer PJ, Weiner CP, Gonik B, eds. High risk pregnancy: Management options (3rd ed). Philadelphia: Elsevier Saunders; 2006. p. :1098-124.
- [Google Scholar]
- Successful pregnancy in a chronically hemodialyzed patient with end-stage renal failure. Indian J Nephrol. 2009;19:27-9.
- [Google Scholar]
- Renal diseases. In: Fleisher LA, ed. Anesthesia and Uncommon Disease (5th ed). Philadelphia, PA: Saunders Elsevier; 2006.
- [Google Scholar]
- Placental transfer and fetal virulence of drugs (in Japanese) Rinsho-Masui. 1991;15:984-92.
- [Google Scholar]
- Safe spinal anesthesia in a woman with chronic renal failure and placenta previa. Int J Gen Med. 2010;31:53-6.
- [Google Scholar]
- Cesarean section under spinal anesthesia for a patient with chronic renal failure. Masui. 1996;45:880-3.
- [Google Scholar]
- Anesthesia for Obstetrics. (3rd ed). Philadelphia: Lippincott Williams and Wilkins; 2002. p. :218.
- [Google Scholar]
- Hepatic drug metabolism and transport in patients with kidney disease. Am J Kidney Dis. 2003;42:906-25.
- [Google Scholar]
- Plasma potassium concentration during N2O-enflurane anesthesia in patients on chronic hemodialysis. Masui. 1993;42:402-5.
- [Google Scholar]
- Serum potassium concentrations after succinylcholine in patients with renal failure. Anesthesiology. 1972;36:142-5.
- [Google Scholar]







