Translate this page into:
Percutaneous renal biopsy in children: Are British Association of Pediatric Nephrology standards achievable?
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
There is considerable variation in the way of preparation and techniques employed for renal biopsy.[1] There are no nationally agreed standards of practice and complications rates for renal biopsies in Indian children. The British Association of Pediatric Nephrology (BAPN) have recently published an audit and laid down standards for renal biopsies in children.[12] This study was aimed to determine the adequacy of percutaneous renal biopsy, its complications with outcome compared with standards laid down by BAPN.
This was a prospective study from June 2010 to September 2012 in a single pediatric nephrology unit of a tertiary care hospital. Intravenous midazolam (0.15 mg/kg) and ketamine (1-2 mg/kg) was used for sedation and local anesthesia was achieved by lignocaine. All biopsies were performed on the lower pole of left kidney under real time ultrasound guidance and with automated spring-loaded biopsy gun (18 G). Children were monitored for 24 h for any other complications. Biopsies were evaluated against the standards of BAPN.[2]
Standards:
-
Adequate tissue for histological diagnosis (on review with histopathologist) in >95% biopsies. Adequacy was defined as >10 glomeruli on light microscopy
-
Number of needle passes to obtain adequate tissue: ≤3 in native kidneys in 80% of patients
-
Major complication rate: <5% (macroscopic hematuria, requirement of blood transfusion, surgical exploration, delay in discharge, readmission).
During the study period, total 57 biopsies were done. Biopsy was diagnostic in 100% of children. The mean glomeruli yield was 17, (range: 8-34) for light microscopy. Tissue was also obtained for immunofluorescence in all cases. Number of needle passes to obtain adequate biopsy material was <3 in 100% of patients. Adequate tissue for histological diagnosis (≥10 glomeruli for light microscopy) was obtained in 96.5% of biopsies. The most common indication for biopsy was steroid-resistant nephrotic syndrome (75%) and minimal change disease (56%) was the most common histology irrespective of the indications for renal biopsy. Major complication in the form of gross hematuria was seen in 3.5% of the patients. None required intravenous fluids, blood transfusions and there were no biopsy site infection or sedation related problems.
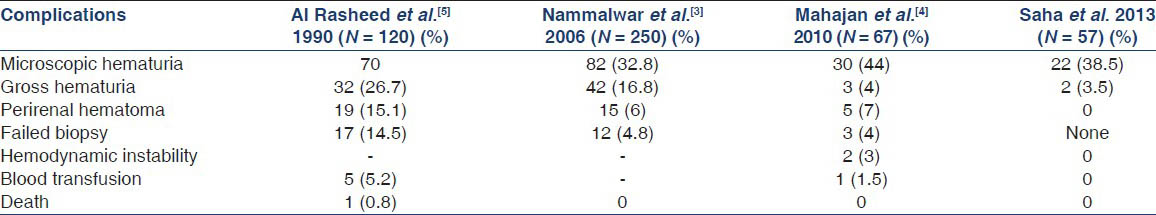
In our study, biopsy was diagnostic in 100% children and inadequate tissue was obtained in 3.5% cases using the adequacy of more than 10 glomeruli for light microscopy. Two previous Indian studies have reported biopsy failure as 4.8% and 4% respectively and adequacy was defined as >5 glomeruli in both studies.[34] All the children, required <3 needle passes for obtaining adequate tissue in our study for histological diagnosis and meet the BAPN guidelines. Perinephric hematoma was reported in 7-15.1% in previous studies;[45] was not seen in any of our cases on ultrasonography [Table 1]. This could be because of a higher proportion of cases of acute kidney injury in the previous study.
Renal biopsy performed in controlled settings under ultrasound guidance has minimal risk of complication and BAPN standards may be achievable.
References
- Renal biopsies in children: Current practice and audit of outcomes. Nephrol Dial Transplant. 2010;25:485-9.
- [Google Scholar]
- Standards for renal biopsies: Comparison of inpatient and day care procedures. Pediatr Nephrol. 2003;18:53-6.
- [Google Scholar]
- Experience of renal biopsy in children with nephrotic syndrome. Pediatr Nephrol. 2006;21:286-8.
- [Google Scholar]
- Should ultrasound guided percutaneous renal biopsy in children be done in a day care setting? Indian J Nephrol. 2010;20:21-4.
- [Google Scholar]
- The outcome of percutaneous renal biopsy in children: An analysis of 120 consecutive cases. Pediatr Nephrol. 1990;4:600-3.
- [Google Scholar]






