Translate this page into:
Depression and anxiety as potential correlates of post-transplantation renal function and quality of life
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The objective of this study was to determine anxiety and depression and its relationship with quality of life (QOL) in renal transplant (RT) recipients. A total of 105 consecutive patients were assessed cross-sectionally at least 3 months after RT. Hospital Anxiety and Depression Scale was applied to assess anxiety and depression. QOL was assessed through the abbreviated version of World Health Organization QOL scale. Patients’ awareness of illness and treatment was assessed through Structured Interview for Renal Transplantation. Nine (8.57%) patients had syndromal anxiety and 9 (8.57%) had syndromal depression. Both these groups had significantly lower scores in almost all domains of QOL compared with their non-anxious and non-depressed counterparts. There were a higher number of hospitalizations and episodes of complication or rejection in post-RT patients with anxiety as compared to those without (P = 0.001). Syndromal depression and anxiety are associated with poor QOL and syndromal anxiety is associated with significantly higher number of hospitalizations, rejections and complications in post-RT patients.
Keywords
Anxiety
depression
outcome
renal function
renal transplantation
Introduction
Renal transplantation (RT) as an effective mode of treatment of end stage renal disease has gained popularity across the world. India has been no different. Compared to hemodialysis (HD), RT provides a much better overall outcome.[1] With technological advances and availability of effective therapy for immunosuppression the life expectancy after RT has gone up. That gives us the opportunity to assess the outcome of these patients more holistically, taking morbidity, capacity of work, general life-style into account over and above life expectancy and renal function estimates. Formerly, transplant outcomes were measured mainly from the perspective of the clinicians, focusing on survival, creatinine values, degree of hypertension and so forth. Now, the subjective experiences of the patients are increasingly recognized as an important outcome measure.[2]
In this regard quality of life (QOL) has been receiving attention of researchers of late. The term QOL refers to the physical, psychological and social domains of health seen as distinct areas that are influenced by patients’ beliefs, experiences, expectations and perception. QOL and psychosocial well-being usually improve after a renal transplant and remain stable for a minimum of several years.[3] Exceptions are often made by non-adherence: the degree to which the patient's behavior differs from agreed medical recommendations. It has been consistently found to affect mortality and morbidity in these patients.[4] Moreover, symptom experience has been shown to be related to non-adherence and health related QOL in renal transplant patients.[5]
Psychological factors, prominent through their presence as comorbidities, are the other sources of concern. Depression,[67] anxiety[8] and alteration of the body image[9] have often been observed as comorbid conditions in patients of RT. These conditions might adversely affect the adherence and thereby undermine effective immunosuppression. Besides that, these conditions also may mar the broader picture of outcome where psychological well-being, satisfaction, capacity to work are considered among others.
Current study addresses these factors in assessing outcome of RT patients. We have assessed the patients cross-sectionally and estimated the renal function along with the level of depression, anxiety, adherence and the overall QOL. The outcome was defined as the composite QOL including physical and psychological well-being. The aim of the current study has been to see if and how the psychological factors as well as the parameters relevant to graft function are associated with the outcome of these patients.
Materials and Methods
Participants
This was a cross-sectional observational study carried out at the transplantation clinic in the Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India. It is a renowned hospital in the country with a wide catchment area including the entire eastern India along with other parts of the country. Ethical clearance was obtained from Institutional ethics committee prior to conducting the study. The study sample consisted of 105 consecutive post-RT patients aged ranges from 18-60 years attending the clinic and fulfilling the inclusion criteria. Written informed consent was obtained from all the participants. Inclusion criteria for the patients were stable clinical condition, absence of any infection or acute complication and an interval of at least 3 months after transplantation. Patients currently admitted in hospital for any reason were excluded.
Tools for assessment
Socio-demographic and clinical data was gathered using a pro-forma specially designed for the study which included all the relevant parameters as described in literature including age, sex, marital status, family type, monthly income, education, residence, current and past employment status, past medical and psychiatric history, family history, current and past intake of psychoactive substance (s) among others. Information related to renal function and transplantation was gathered from hospital charts. These included duration of renal failure, native kidney disease (whenever the information is available), duration and type of dialysis, complications (if any) and general health during dialysis, creatinine level and medications immediately after transplantation (after discharge from the hospital) as well as on current assessment, episodes of rejection, infection, hospitalization, new onset diabetes after transplantation (NODAT) if any, cost of treatment, etc. Patients’ understanding of the current treatment and course of recovery after transplantation was assessed through a list of questions cited in the Structured Interview for Renal Transplantation (SIRT)[10] which assesses patient's ability to identify medications, state the purpose of transplantation, the side-effects of medications, the symptoms and risk of rejection, the importance of compliance and the post-operative recovery course. Anxiety and depression were assessed by Hospital Anxiety and Depression Scale (HADS).[11] This scale consists of 14 items, seven each to assess depression and anxiety. Each item has a maximum score of 3. Scores of ≥11 on either depression or anxiety denotes significant psychological morbidity.[12] Adherence was assessed by Morisky's eight item Medication Adherence Scale[13] with relevant modifications. This scale was devised to check adherence in patients with hypertension. So, few modifications were made before using it in the current study, e.g., the expressions such as “blood pressure treatment plan” was replaced by “treatment plan” or “blood pressure medicine” was replaced by “medicine”. The questions in this scale are relevant to the current research and it has the added advantage of being brief and focused. The maximum obtainable score in this scale is 8 which denotes high adherence, a score below 6 denotes low adherence and scores between 6 and 8 is considered medium adherence. QOL was assessed through the abbreviated version of World Health Organization (WHO) QOL scale (WHOQOL-BREF).[14] It is a 26-item questionnaire which is scored on a Likert scale from 1-5 and generates four domain scores.
Procedure
All the rating scales were administered on the patients during clinical visit to the transplantation clinic. The assessments were done by the first author, AKJ.
Statistical analysis
The collected data was statistically analyzed using Statistical Package for Social Sciences (SPSS) 16.0 for Windows. Based on HADS subscale score (11 or more or <11), patients were grouped as with or without anxiety and depression. The groups were compared using Mann-Whitney U-test and Fisher's exact test for continuous and categorical variables, respectively. The effect sizes were reported as r (calculated from z value of Mann-Whitney U-test)[15] and Cramer's V. The level of significance was set at P < 0.05 (two-tailed).
Results
The mean age of the sample was 35.03 [standard deviations (SD) 9.75] years and mean years of education was 12.2 (SD 3.15) years. Among them 76 (72.4%) were males, 67 (63.8%) were married and 53 (50.5%) were employed. The median duration of renal failure was 12 [interquartile range (IQR) 15] months and median duration of dialysis was 6 (IQR 5) months. The median time elapsed since transplantation was 23 (IQR 32) months.
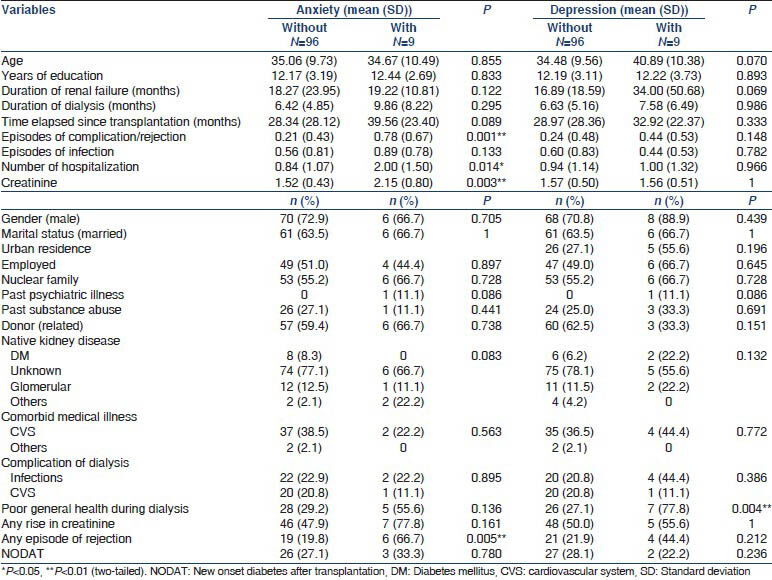
Among the patients, 9 (8.57%) had depression and 9 (8.57%) had anxiety as assessed by HADS. The mean HADS depression and anxiety score in these patients was 12.78 (SD 2.22) and 10 (SD 5.77), respectively. The comparisons of socio-demographic and clinical variables among the groups are summarized in Table 1. There were significantly higher number of episodes of complication or rejection in post-RT patients with anxiety as compared to those without (U = 223, z = −3.23, P = 0.001, r = 0.32). Furthermore, the post-RT patients with anxiety had significantly higher number of hospitalizations than those without anxiety (U = 232, z = −2.45, P = 0.014, r = 0.24). There was significantly lower creatinine levels in those without anxiety as compared to those with anxiety disorder (U = 176, z = −2.93, P = 0.003, r = 0.29). Significantly higher number of post-RT patients without depression had a poor general health (78%) during dialysis compared to their counterparts (27%) with depression (P = 0.004, Cramer's V = 0.31). In those with anxiety, 70% had any episode of rejection as compared to only 20% without anxiety, which was statistically significant (P = 0.005, Cramer's V = 0.31). For post-RT patients with depression the mean age was higher and mean duration of renal failure was longer than the patients without depression but for both these parameters the differences did not reach statistical significance though a trend could be noticed in both cases.
The differences between patients with depression or anxiety and those without in various domains of QOL, adherence as well as in their awareness of the current treatment and course of recovery are summarized in Table 2. In those with anxiety, QOL was significantly lower in four out of five domains, i.e., “general” (U = 60, z = −4.39, P < 0.001, r = 0.43), “experience” (U = 175.5, z = −2.95, P = 0.003, r = 0.29), “satisfaction” (U = 75.5, z = −4.13, P < 0.001, r = 0.40) and “depression” (U = 108, z = −4.03, P < 0.001, r = 0.39), whereas it was not significantly different in “ability” domain. In patients with depression, QOL was significantly lower in all domains, i.e., “general” (U = 163.5, z = −3.17, P = 0.002, r = 0.31), “experience” (U = 109.5, z = −3.71, P < 0.001, r = 0.36), “ability” (U = 230.5, z = −2.33, P = 0.02, r = 0.23), “satisfaction” (U = 134.5, z = −3.41, P = 0.001, r = 0.33) and “depression” (U = 87, z = −4.29, P < 0.001, r = 0.42).

Discussion
The present study examined 105 consecutive RT patients fulfilling the criteria and assessed their comprehensive renal function through reviewing charts and their awareness about treatment and illness along with its course through a validated instrument [Structured Interview for Renal Transplantation (SIRT)] made solely for this purpose. The assessments of their anxiety, depression and QOL were made with the help of another set of validated and standardized instruments (HADS and WHOQOL-BREF). A study of this sample size with meticulous assessments of their renal function as well as psychiatric comorbidity has not been carried out so far from this part of the world. Our study reveals a point prevalence of both syndromal anxiety and depression to be 8.57% each (nine patients out of 105). The presence of anxiety and depressive symptoms in a sub-syndromal level is more widespread among the post-RT subjects. Alavi et al.[16] in their cross-sectional study of 100 RT and 63 HD patients had shown 65.3% and 51.6% of the RT patients had depression and anxiety respectively using Symptom Checklist-90 subscales of depression and anxiety. Whereas 24 out of 88 (27.27%) patients had anxiety and 20 out of 88 (22.73%) had clinical depression in another study[17] in Iran where, like the current study, the assessments were made using HADS and cases were defined when the scores exceeded 11. An even higher prevalence (anxiety in about 50% and depression in 25% of patients) has also been reported from Turkey.[8] These differences in prevalence across studies might reflect the inherent differences of the study groups as prevalence of depression is known to vary widely across nations.[18]
A somewhat unexpected finding was that a significantly higher number of patients without depression had a poor general health during dialysis than their depressed counterparts. The reports of general health prior to RT while patients were on HD were gathered from the patients themselves based on their recall. The “general health” was assessed through General Health Questionnaire-12[19] and a score of over 3 was considered poor general health. This is a reflection of health prior to RT and the depression that was assessed in the current study developed after RT with possible psychosocial as well as biological causes underlying it. Therefore, a higher number of non-depressed patients showing poor general health do not produce any serious incongruity to the overall study findings.
Another surprising finding was neither anxiety nor depression was seen to be associated with poor adherence. It is general wisdom among psychiatrists that adherence is a big challenge in treating any of the psychiatric disorders. Depression has specifically been shown to negatively affect immunosuppressive medication adherence in a previous study.[20] However, in the current study neither anxiety nor depression was seen to be associated with poor adherence. This may be due to the low prevalence of psychiatric comorbidity detected in the current study thereby not adequately reflecting the picture of adherence in RT patients. Another possible explanation is that the patient education delivered by all the members of the transplantation clinic during the attendance of patients in the clinic through individual and group counseling might have improved compliance.
As expected, the various domains of QOL were poor in patients with anxiety and depression. Patients with depression had a significantly poorer QOL in all domains in comparison with the patients without depression with medium effect sizes for most of the subscales. For patients with anxiety, however, there was not any significant difference in the subscale of “ability” in comparison with their non-anxious counterparts. QOL in its various domains as well as the perception of QOL have been shown to be poor in RT patients with depression.[17]
The post-RT patients with anxiety had significantly more episodes of complications or rejections with a medium effect size (r = 0.32) and higher number of hospitalizations with a small effect size (r = 0.24) compared to their non-anxious counterparts. Futhermore, among those with anxiety the proportion of subjects with any episode of rejection (70%) was significantly higher than among those without anxiety (20%) and the effect size of this difference was medium (Cramer's V = 0.31). Another important finding was that the creatinine level was significantly lower in patients without anxiety compared to their anxious counterparts though the effect size was small (r = 0.29). These findings in the current study show anxiety being related to parameters directly reflecting post-RT renal function. Such findings have not been reported in any of the previous studies. In a previous study, Noohi et al.[17] compared the patients with syndromal anxiety against those with sub-syndromal anxiety and could not spot any significant difference in the history of graft rejection. There has been a concern among the researchers about the presence of psychiatric disorders in RT patients as these conditions might increase the morbidity. Since a process of RT is not just aimed at patient survival, but also at decreasing the morbidity to a minimum, a parallel assessment of these conditions is considered useful. Furthermore, the current study showed that a psychiatric comorbidity in the form of anxiety, was not just leading to a poor QOL, but also was associated with episodes of graft rejection, complications, higher level of creatinine and more number of hospitalizations, i.e., the parameters more closely reflecting renal function after RT per se.
The major limitation of our study was the cross-sectional design. A longer period of observation would have given us a better picture of the role of psychiatric morbidity in post-RT renal function and overall outcome. Furthermore, assessment of biological parameters such as cortisol level, could possibly suggest a link between the stress arising out of RT and the development of psychiatric comorbidities. This also limits the study as a hypothesis on the possible causes of psychiatric comorbidities could not be proposed. Furthermore, Medication Adherence Scale has not been validated in post-RT patients, which limits its use in this population. Future studies addressing these limitations might come out with more interesting findings.
Source of Support: Nil
Conflict of Interest: None declared.
References
- The adjustment to illness in patients with generalized anxiety disorder is poorer than that in patients with end-stage renal disease. J Psychosom Res. 2004;57:165-70.
- [Google Scholar]
- Incorporating the patient's perspective into drug development and communication: An ad hoc task force report of the Patient-Reported Outcomes (PRO) Harmonization Group meeting at the Food and Drug Administration, February 16, 2001. Value Health. 2003;6:522-31.
- [Google Scholar]
- Changes in quality of life after renal transplantation. Am J Kidney Dis. 1998;32:93-100.
- [Google Scholar]
- Frequency and impact of nonadherence to immunosuppressants after renal transplantation: A systematic review. Transplantation. 2004;77:769-76.
- [Google Scholar]
- Patient noncompliance: A major cause of late graft failure in cyclosporine-treated renal transplants. Transplant Proc (20 Suppl 3):63-9.
- [Google Scholar]
- Depression levels before and after renal transplantation. Transplant Proc. 2004;36:111-3.
- [Google Scholar]
- Depressive disorder in renal transplantation: An analysis of Medicare claims. Am J Kidney Dis. 2008;51:819-28.
- [Google Scholar]
- Cross-sectional assessment of psychiatric disorders in renal transplantation patients in Turkey: A preliminary study. Transplant Proc. 2004;36:1419-21.
- [Google Scholar]
- Changes in quality of life after renal transplantation. Transplant Proc. 2005;37:1618-21.
- [Google Scholar]
- The structured interview for renal transplantation-SIRT. Psychosomatics. 2000;41:393-406.
- [Google Scholar]
- The influence of anxiety, depression and post traumatic stress disorder on quality of life after thoracic organ transplantation. Z Psychosom Med Psychother. 2003;49:262-74.
- [Google Scholar]
- Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348-54.
- [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF quality of life assessment The WHOQOL Group. Psychol Med. 1998;28:551-8.
- [Google Scholar]
- Depression, anxiety, activities of daily living, and quality of life scores in patients undergoing renal replacement therapies. Transplant Proc. 2009;41:3693-6.
- [Google Scholar]
- Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proc. 2007;39:1074-8.
- [Google Scholar]
- Understanding cross-national differences in depression prevalence. Psychol Med. 2002;32:585-94.
- [Google Scholar]
- Depression and immunosuppressive medication adherence in kidney transplant patients. Gen Hosp Psychiatry. 2008;30:386-7. 20
- [Google Scholar]







