Translate this page into:
Obstructive uropathy: Is it always urolithiasis?
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 54-year-old diabetic female was admitted with left lank pain and high grade fever since 4 days. Ultrasonography showed left hydronephrosis with proximal ureteric dilatation. The patient was treated with intravenous broad spectrum antibiotics and her sugar levels optimized. Urinanalysis showed field full of pus cells. The renal function tests were deranged (blood urea 84 mg/dl, serum creatinine 2.1 mg/dl). Total leukocyte counts were 18,000/mm3. Noncontrast computed tomography (CT) scan KUB showed a radiodense shadow at the level of L3 vertebrae in left ureter causing proximal hydroureteronephrosis [Figure 1]. The patient was posted for uretero-renoscopic lithotripsy of the calculus. However, on ureteroscopy a necrosed renal papilla was found impacted in the proximal ureter [Figure 2a]. It was removed and a Double J stent was placed. The necrosed papilla with calcification was confirmed on histopathologic examination [Figure 2b]. The total white blood cells counts reduced to normal limits on 1st postoperative day (POD) and she was discharged on POD 2 on oral antibiotics.

- A coronal image showing a radio dense shadow in left proximal ureter
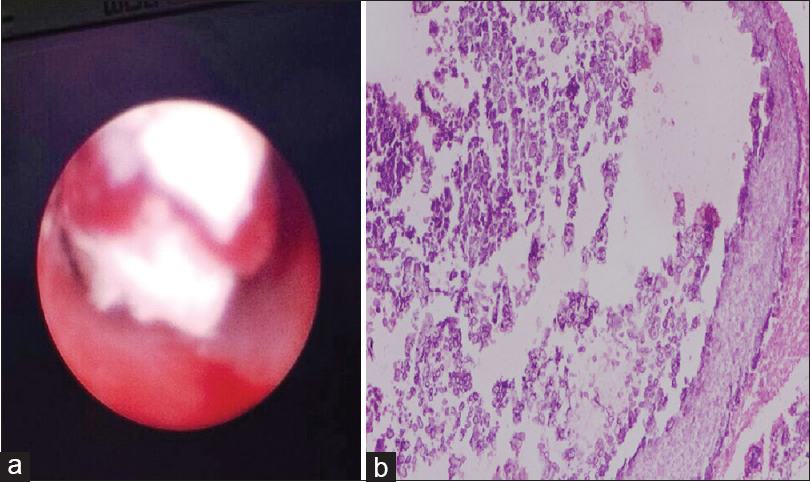
- (a) An endo-urologic view of the necrosed papilla in ureter. (b) A microscopic view of papilla showing crystalline material embedded in amorphous background tissue
Renal papillary necrosis (RPN) is a clinical condition that arises due to impairment of blood circulation to papillary tip of renal medulla due to diabetes mellitus, sickle cell disease, pyelonephritis, renal vein thrombosis, analgesic abuse, genitourinary tuberculosis and obstructive uropathy. In many situations, these clinical conditions might be found in isolation or in combination with each other. Renal allograft (cadaver donor more than live donor) after kidney transplantation is also prone to this condition[12] owing to acute rejection due to fungal infections.[34]
The diagnosis of RPN remains challenging. Previously, intravenous urography was commonly performed in such situation. In recent times, CT urography has proved to be much more informative in diagnosing RPN. Thinner sections, and reconstructed imaging with multidetector row CT has further taken us a step closer in documenting this condition.[56] Necrosed renal papilla might get calcified prior to detachment and subsequently lead to obstructive uropathy after getting impacted anywhere in ureter. Ultrasound at this point, followed by CT KUB might easily give a false impression of a ureteric calculus causing obstruction, as presented in a given scenario.
References
- Papillary necrosis causing hydronephrosis in the renal allograft. Sonographic findings. J Ultrasound Med. 1989;8:579-81.
- [Google Scholar]
- Papillary necrosis following segmental renal infarction: An unusual cause of early renal allograft dysfunction. Nephrol Dial Transplant. 2005;20:830-3.
- [Google Scholar]
- Isolated urinary aspergillosis in a renal transplant recipient. Nephrol Dial Transplant. 1998;13:2382-4.
- [Google Scholar]
- Computed tomographic diagnosis of ureteral obstruction caused by a sloughed papilla. Urol Radiol. 1987;9:45-6.
- [Google Scholar]
- Multi-detector row CT urography in the evaluation of hematuria. Radiographics. 2003;23:1441-55.
- [Google Scholar]






