Translate this page into:
Endovascular embolization of pseudoaneurysm of left colic artery developing after renal biopsy
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vascular complications after percutaneous renal biopsy are uncommon and may require interventional management. In most of these cases, the pathology is a renal arterial pseudoaneurysm (PsA) or an arterio-venous fistula. Injury to other vessels like aorta, lumbar arteries or mesenteric arteries is rare with only one case of left colic artery PsA reported in literature. We report a case of a 60-year-old female, who developed left colic artery PsA after renal biopsy, which was successfully embolized through endovascular route using microcoils.
Keywords
Embolization
left colic artery
pseudoaneurysm
renal biopsy
retroperitoneal hematoma
Introduction
Vascular complications after percutaneous renal biopsy are uncommon with macroscopic hematuria occurring in up to 3.5% of patients.[1] Most are self-limited with blood transfusion needed in only about 0.9% and radiologic intervention in 0.6% cases.[1] The pathology seen on angiography in most cases is either renal arterial pseudoaneurysm (PsA) or arterio-venous fistula (AVF). Rarely, aorta, lumbar artery and superior mesenteric artery may be injured during biopsy.[2345] But injury to left colic artery is very rare with only one case reported in literature.[6] We report a case of left colic artery PsA developing after renal biopsy, which was successfully embolized using microcoils.
Case Report
A 60-year-old female presented to the nephrology outpatient clinic with history of pedal edema and periorbital swelling and abdominal distension of 3 months duration. No history of diabetes mellitus or hypertension was present. Clinical examination was unremarkable. Lab investigation revealed blood urea of 124 mg/dl, serum creatinine of 3.5 g/dl and estimated glomerular filtration rate of 35 mL/min/1.73 mm2. Ultrasonography revealed normal sized bilateral kidneys with increased echogenicity and effacement of corticomedullary differentiation. There was no hydronephrosis. Subsequently a renal biopsy was done in the nephrology ward by conventional technique (without ultrasound guidance). After renal biopsy, she developed abdominal pain and gradually increasing swelling in left flank region. There was no hematuria. The patient's monitor revealed tachycardia (pulse rate 132/min) and low blood pressure (100/70 mm Hg). Fluid resuscitation was started immediately. Her hemoglobin level dropped from 12.5 g/dl to 8 g/dl. Ultrasonography showed a large heteroechoic area around the left kidney suggesting perinephric hematoma. There was no obvious PsA in the left kidney. With a suspicion of renal artery PsA, digital subtraction angiography (DSA) of left renal artery was done. The renal arteries were normal and no PsA or AVF was seen.
When even after 48 h patient's symptoms did not improve, computed tomography (CT) angiography was done, which showed a large hematoma in the left retroperitoneal region and a PsA arising from a branch of inferior mesenteric artery [Figure 1]. The PsA was not seen in the arterial phase and was better seen on the venous phase due to its narrow neck. The patient was immediately shifted to angiography suite and DSA was done through transfemoral route. Inferior mesenteric artery DSA showed the PsA arising from the ascending branch of left colic artery [Figure 2a and b]. A 2.7 Fr microcatheter was used to reach distal to the neck of PsA and the segment adjacent to the neck of PsA was embolized using microcoils. Post embolization, DSA showed no opacification of the PsA [Figure 2c]. The vascular arcade supplying the colon showed normal opacification through collaterals. Within few hours after the procedure, the patient's vital parameters improved. No symptoms of colonic ischemia appeared. Subsequently the patient remained stable without any drop in hemoglobin levels.
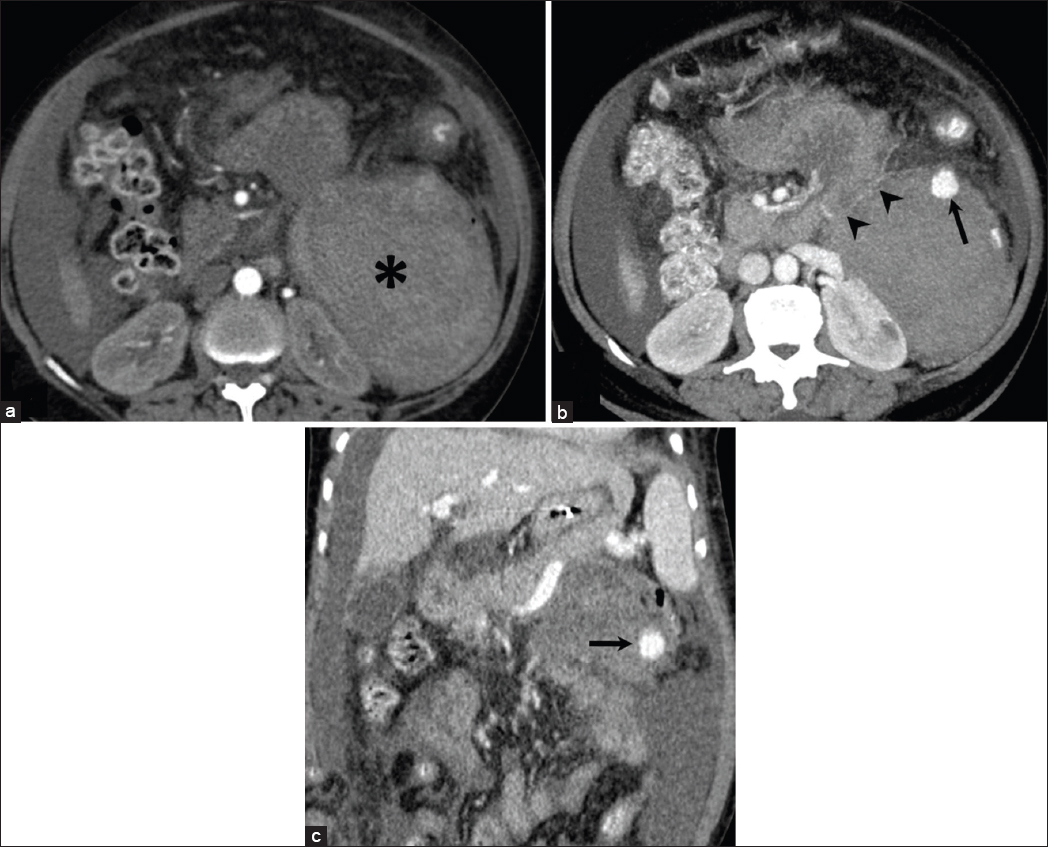
- (a) Arterial phase computed tomography (CT) scan shows a large hematoma (*) in the left anterior pararenal space. The pseudoaneurysm (PsA) was not seen. (b) Axial and (c) Coronal CT images in venous phase shows the enhancing PsA on the anterior aspect of the hematoma (arrow). An attenuated artery is seen feeding the PsA (arrow heads)
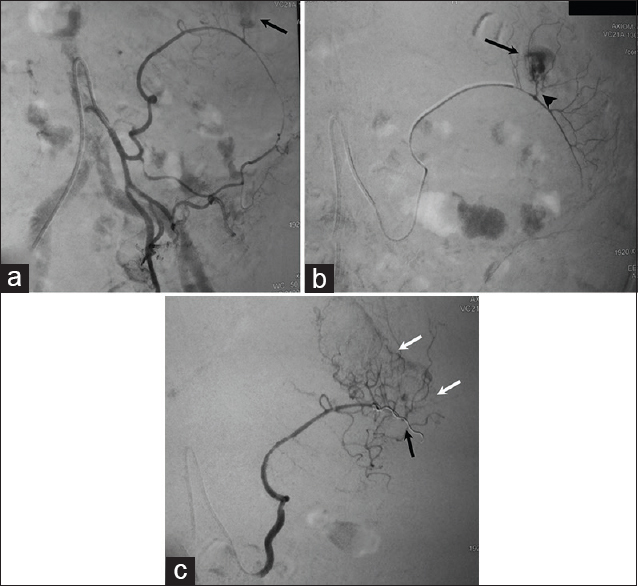
- Digital subtraction angiography. (a) Inferior mesenteric artery angiogram shows pseudoaneurysm (PsA) arising from the left colic branch (arrow; PsA not fully included in the frame). (b) Selective angiogram with microcatheter shows the narrow neck (arrow head) of the PsA (arrow). (c) Angiogram after placement of microcoils (black arrow) shows complete embolization of the PsA. Vascular arcade of the colon is preserved, seen through collateral circulation (white arrows)
Discussion
Percutaneous renal biopsy, when done under ultrasonographic guidance, is rarely associated with complications. Perinephric or retroperitoneal hematoma is seen in up to 17% patients when an ultrasonography is done in post-biopsy period.[1] Higher rates of bleeding are seen with the use of larger bore needles, higher serum creatinine values and presence of acute kidney injury.[1] Most of the complications resolve with conservative management. The incidence of PsA and AVF developing after percutaneous renal biopsy is rare, occurring in about 1–2% cases.[7] Most of these patients present with hematuria, pain and swelling. Most of the AVFs remain asymptomatic or resolve spontaneously on follow-up, and intervention is necessary only if they become symptomatic.[78]
Pseudoaneurysms developing after renal biopsy are very rare, although exact incidence is not known in literature. As with other PsA, renal PsA are also unstable and may often rupture into the pelvicalyceal system or perinephric space resulting in hematuria or hematoma. Hence, these need to be treated to avoid life-threatening hemorrhage. PsA of extra-renal arteries are very rare, with a few case reports of injury to aorta, superior mesenteric artery, lumbar artery and left colic artery. Only two of these reported cases were successfully embolized endovascularly.[26] Involvement of left colic artery has been reported only once in English literature.[6] The left colic artery arises from the inferior mesenteric artery and divides into ascending and descending branches and the former courses anterior to the left kidney toward the descending colon and anastomoses with the branches of middle colic artery and first sigmoid artery to form the vascular arcade.[9] Due to its location close to left kidney, it may rarely be at risk of injury during biopsy, especially when biopsy is done without guidance.
The patients of extra-renal arterial involvement develop retroperitoneal hematoma or hemoperitoneum rather than hematuria and may present with hypotension, pain/swelling and/or drop in hemoglobin.[23456] Although ultrasonography with color Doppler may be useful in some cases, most of the patients with persistent symptoms beyond 24–48 h need CT angiography for evaluation of renal and extra-renal arteries. Adequate precautions are needed while performing CT scan as iodinated contrast may further deteriorate the already compromised renal function. These include adequate hydration, use of iso-osmolar contrast agent and to perform hemodialysis after the scan. CT angiography will demonstrate any PsA or AVF and/or any leak of contrast and also helps in providing a road map for angiography and embolization. DSA can also be done as a first line of investigation without CT angiography as catheterization and angiography of the renal artery will provide information about the abnormality better than CT scan and also allows embolization in the same sitting. Also, it helps in avoiding additional dose of iodinated contrast agent used in CT scan. However, if small accessory renal or extra-renal artery is the source of bleed, it may be missed, as angiogram of only renal artery of the involved kidney is done and it would be a tedious process to search for other arteries.
Digital subtraction angiography should be done with minimum amount of iodinated contrast agent. Carbon-dioxide can also be used as contrast agent. Superselective catheterization of the branch/artery supplying the PsA must be done for better demonstration of neck of PsA and for successful embolization with minimal complications. Embolization agent most widely used is coil/microcoil. As the renal artery is an end artery, embolizing the feeding arterial branch with coil is sufficient for obliterating the PsA. However, in case of mesenteric arteries, due to collateral supply, occlusion of distal and proximal segment across the neck of PsA is needed for successful embolization. Also, coil embolization of shortest segment of the mesenteric artery feeding the PsA prevents ischemia to the bowel due to collateral circulation.[10] In our case, we initially did not expect extra-renal artery involvement and hence we performed left renal DSA without CT angiography to avoid administering higher iodine contrast and contrast induced nephropathy. But since the patient did not improve, CT angiography was needed which showed PsA from left colic artery, which was successfully embolized using microcoils. However, such complications are very rare and CT angiography as first line of investigation should be done only in selected patients.
Conclusion
Extra-renal artery PsA after renal biopsy is extremely rare and should be considered in a patient with retroperitoneal hematoma and without hematuria. Direct DSA of renal arteries may miss these lesions and CT angiography is informative.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Bleeding complications of native kidney biopsy: A systematic review and meta-analysis. Am J Kidney Dis. 2012;60:62-73.
- [Google Scholar]
- Massive hemorrhage from a lumbar artery following percutaneous renal biopsy. Am J Kidney Dis. 1986;7:250-3.
- [Google Scholar]
- Life-threatening hemorrhage from abdominal aorta following a percutaneous renal biopsy. Clin Nephrol. 2006;65:446-8.
- [Google Scholar]
- Laceration of a mesenteric artery: Unusual complication of percutaneous renal biopsy. South Med J. 1980;73:1413-4.
- [Google Scholar]
- Severe haemorrhage from a lumbar artery as a complication of percutaneous renal biopsy. Postgrad Med J. 1985;61:69-70.
- [Google Scholar]
- Life-threatening intra-abdominal hemorrhage from left superior colonic artery pseudoaneurysm after percutaneous renal biopsy: Successful treatment with superselective arterial embolization. Clin Imaging. 2009;33:474-7.
- [Google Scholar]
- Doppler US evaluation of renal biopsy complications in children. Diagn Interv Radiol. 2013;19:15-9.
- [Google Scholar]
- Renal biopsy in high-risk patients with medical diseases of the kidney. Am J Kidney Dis. 2000;36:419-33.
- [Google Scholar]
- Gray's Anatomy: The Anatomical Basis of Clinical Practice. London: Churchill Livingstone; 2008.
- [Google Scholar]







