Translate this page into:
Adequacy of twice weekly hemodialysis in end stage renal disease patients at a tertiary care dialysis centre
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hemodialysis has improved the morbidity and mortality associated with end stage renal disease. In India, hemodialysis prescription is empiric, which leads to complications related to under-dialysis. Hence, adequacy of hemodialysis in Indian setting was analyzed in this study. A total of 50 patients on twice per week hemodialysis were assessed for 1 month. The number of sessions meeting standards laid out by Kidney Diseases Outcome Quality Initiatives (KDOQI) guidelines were calculated. They were divided into two groups: one in whom dialysis was monitored and session length enhanced to meet the minimum standard Kt/V of 2 and second control group; where Kt/V was not monitored. Hemoglobin (Hb) levels, albumin levels, mean arterial pressure and World Health Organization (WHO) quality of life (QoL) score were compared in the two groups after 6 months. Only 28% of hemodialysis sessions were adequate as per KDOQI guidelines. There was significant improvement in Hb levels (1.47 vs. 0.15 g/dl), mean arterial pressure levels (15.2 vs. 3.16 mm Hg), serum albumin levels (0.82 vs. 0.11 g/dl) and WHO QoL score (17.2 vs. 2.24) in study group as compared to control group. Standard Kt/V can be used as an important tool to modify twice weekly dialysis sessions to provide better QoL to the patients. However, studies with larger sample size are required to conclusively prove our results.
Keywords
End stage renal disease
hemodialysis adequacy
hemodialysis frequency
Introduction
Chronic kidney disease (CKD) is a devastating disease with profound physical morbidity associated with financial, social and emotional stress on the individual. The definition of CKD is based on the presence of kidney damage (i.e., albuminuria) or decreased kidney function (i.e., glomerular filtration rate <60 mL/min/ 1.73 m2) for 3 months or more. The term “end- stage renal disease” (ESRD) generally refers to CKD treated with either dialysis or transplantation. The age-adjusted incidence rate of ESRD in India has been estimated to be 229/million population.[1] Diabetes is the main cause of kidney failure in most countries, accounting for 40% or more of new patients.[2] Prevalence seems to be increasing particularly in older individuals, and partly because of an increasing prevalence of diabetes and hypertension.[3] Costs for dialysis and transplantation are increasing alongside costs for other chronic diseases.[4]
Hemodialysis is the mainstay therapy which is offered for ESRD patients who cannot undergo renal transplantation. The main purpose of hemodialysis is the provision of sufficient and safe patient treatment, which contributes to the better physical condition of the patient and it prevents further problems and complications that are due to uremia. In India, usually hemodialysis prescription is empiric, which may lead to under dialysis and related complications.[5] The delivered Kt/V determined by single-pool urea kinetic modeling continues to be preferred as the most precise and accurate measure of dialysis. A central issue in the management of patients undergoing maintenance hemodialysis is the assessment of the adequacy of dialysis.
The delivered dose of HD for patients with established renal failure has increased over the last decade.[6] Despite its dramatic success at saving lives, hemodialysis remains far from perfect therapy. More than 20% of hemodialysis patients die each year.[7] In addition, morbidity remains high, with frequent complications of heart disease, hypertension, anemia, bone disease, poor nutrition, inflammation, depression, and impaired cognitive and physical function. In developed countries usually hemodialysis is done thrice a week. However in India most patients are given HD twice a week. Only 20% of patients are dialyzed 3 times a week. The dialysis prescription is empirical, with Kt/V < 1 in the most of patients.[8] Although it is well-known that increasing the frequency of dialysis improves the quality of life (QoL), it is not an option due to pressure from too many patients and inadequate hemodialysis machines.
While optimal levels remain to be established, doses of dialysis represented by Kt/V measurements <1.20 are widely considered inadequate.[9] Below this level, each 0.10 decrease in Kt/V is estimated to increase the relative risk of death by 7%.[10] The standardized Kt/V is a method to measure the clearance efficiency of HD of variable frequency, slow continuous renal replacement therapies, residual renal function (RRF) and all situations involving the use of clearance from various methods.[11] The serum albumin concentration, which is used routinely as a marker of nutritive status, is the result of the synthesis, catabolism and volume re-distribution, as well as trans capillary exchange loss.[12] World Health Organization (WHO) QoL BREF score provides a measurement of functioning and well-being rather than of diseases and disorders, hence is more comprehensive and compatible with the WHO's concept of health.[13] This score can act as an outcome measure to compare management strategies.[14]
Hemodialysis Adequacy Clinical Practice Guidelines 2006 recommends spKt/V of 2 (minimum spKt/V corresponding to a standardized Kt/V of approximate 2.0/week). For twice a week hemodialysis: If RRF (Kr) >2 mL/min/1.73 m2 the minimum spKt/V should be 2. If Kr < 2 mL/min/1.73 m2 then twice a week hemodialysis is not usually recommended. These spKt/V values need to be considered as minimum values, not target values.
This study is aimed to assess the adequacy of hemodialysis provided at Tertiary Care Center as well as to determine whether adjusting only the duration of dialysis based on standardized Kt/V measurement improves the QoL of patients.
Materials and Methods
Fifty patients on maintenance hemodialysis at a Tertiary Care Center were studied for adequacy of hemodialysis.
Inclusion criteria
-
Patients on maintenance hemodialysis for at least 6 months duration
-
Age >18 years; and <65 years.
Exclusion criteria
-
Patients with acute illness not related to CKD requiring hospitalization in last 1 month
-
Patients on thrice per week hemodialysis
-
Patients on continuous ambulatory peritoneal dialysis.
Methodology
First phase of the study (assessing adequacy of dialysis). Baseline data including basic disease, duration of hemodialysis, height, weight, pulse and blood pressure was recorded. The pre and postdialysis blood urea nitrogen, postdialysis weight and ultrafiltrate volume of 50 patients was recorded weekly for 1 month.
We used the slow blood flow sampling technique[15] for post hemodialysis samples. The spKt/V and eqKt/V was estimated from the pre and postdialysis blood urea nitrogen, postdialysis weight and ultrafiltrate volume using the Davita web based calculator at http://www.davita.com/tools/ktvcalculator. For each week, standard Kt/V was calculated from the spKt/V, average session length, number of sessions of dialysis per week using the HDCN web calculator at http://www.hdcn.com/calcf/ley.htm. The number of sessions meeting standards laid out for adequacy of dialysis as per kidney diseases outcome quality initiatives (KDOQI) guidelines and frequent hemodialysis network was calculated. In the second phase of the study, the 50 patients were randomized into the study group A and control group B after informed consent by computer generated randomization. At baseline clinical parameters, hemoglobin (Hb), serum albumin and the questionnaire based WHO QoL score were recorded in all patients. Thereafter, in the 25 patients in study group A, standardized Kt/V was measured weekly. The length of the dialysis was prolonged if required, to meet a target of two for standardized Kt/V. In the control group, no monitoring of Kt/V was done. After 6 months again clinical parameters, Hb, serum albumin and the QoL questionnaire along with the measures of adequacy of hemodialysis were recorded.
Statistical analysis was performed between the two groups using Mann–Whitney test for differences in Hb levels, albumin levels, clinical parameters and WHO QoL scores. First phase was cross-sectional descriptive study and the second was randomized case–control study. Study was done at a Tertiary Care Dialysis Center. Ethical approval was obtained by ethical committee. Patients' written informed consent was taken in a language that they understand.
Results
Participants
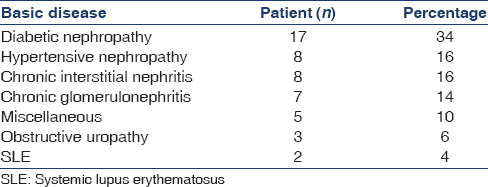
In our study, 56% (n = 28) of the study population was male and 44% (n = 22) was female. The average age of enrolled patients was 56.02 ± 9.89 years (range: 29–65 years). The most common basic disease was diabetic nephropathy; seen in 34% (n = 17) of patients [Table 1].
Mean arterial pressure of our patients (n = 50) was 117.16 ± 10.79 mm Hg (Range: 146–90 mm Hg). Mean Hb level of the study population was 8.15 ± 1.49 g/dl (Range: 12.0–6.4 g/dl). The average albumin levels of our patients (n = 50) was 3.28 ± 0.46 g/dl (Range: 5.5–2.4 g/dl). 82% (n = 41) patients had serum albumin levels <3.5 g/dl. Mean QoL score was 80.78 ± 14.76 (Range: 110–51).
The number of sessions meeting standards laid out for adequacy of dialysis
Totally 400 sessions were analyzed. As per KDOQI guidelines, (minimum standardized Kt/V –2.0, single pool Kt/V −2.0) 112 sessions were found to be inadequate. The average standardized Kt/V was 1.4 [Figure 1].

- Frequency of adequate dialysis sessions (spKt/V > 1.2); total sessions = 400; inadequate sessions = 288 (72%) and adequate dialysis sessions = 112 (28%)
Baseline comparison of both groups with respect to parameters
Both the study groups were approximately matched for age, sex, mean arterial pressure, Hb, albumin and WHO QoL score [Figure 2].

- Baseline comparison of both groups; group A (n = 25). The dialysis sessions monitored and modified as per Kt/V; group B (n = 25) continued on conventional 4 h dialysis sessions twice per week
Difference between study and control group at 6 months follow-up
The average hemodialysis duration in study group (group A) was 318.22 ± 34.11 (range: 240–360) min. In group B, the average duration was 240 ± 30 min [Figure 3].

- Bar diagram depicting change in all parameters. Significant improvement in group A (dialysis sessions monitored and modified as per Kt/V) as compared to group B (continued on conventional 4 h dialysis sessions twice per week)
The average fall of mean arterial pressure in group A was 15.2 ± 7.96 (range: 33.0 to −2.0) mm Hg, whereas in group B it was 3.16 ± 6.84 (range: 28.0 to −7.0) mm Hg. The difference was statistically significant with Mann–Whitney test (P < 0.05). The increase in Hb in group A was 1.47 ± 1.06 (range 3.2–0.1) g/dl as compared to 0.15 ± 0.65 (range: +2.0 to − 1.0) g/dl in group B, which was statistically significant with Mann–Whitney test. The increase in serum albumin was 0.82 ± 0.51 (range: 2.0–0.1) g/dl in group A as compared to 0.11 ± 0.39 (range +1.0 to − 0.5) g/dl in group B (P < 0.05). The average rise in WHO- QoL score was 17.2 ± 11.35 (range: +40 to + 2) in group A as compared to 2.24 ± 8.53 (range: +22 to −12) in group B (P < 0.05). There was a significant improvement in all parameters in study group as compared to the control group [Table 2].

Discussion
At the end of phase I, in our study it was found that 34% of patients had diabetic nephropathy as basic disease. 16% had hypertensive nephropathy, 16% had chronic interstitial nephritis, and 14% had chronic glomerulonephritis. Approximately similar results have been seen in other studies from India such as study by Rajapurkar et al.[16] in 2012. In our study, 84% (n = 42) of patients had Hb levels of <10 g/dl. In our study, the average Hb at onset of the study was 8.1 g/dl. In a study in USA by Reddan et al.[17] in 2003 on patients on thrice per week hemodialysis the average Hb was 11.1 g/dl. Lower Hb levels; seen in our study can be attributed to comparative lower nutritional status, twice a week dialysis, inadequate dialysis and poor compliance with drugs. It was found out that only 28% of hemodialysis sessions were minimally adequate as per KDOQI standards. The average standardized Kt/V was 1.4. This is not a surprising finding as deficient resources and excessive patients per dialysis machine can frequently lead to inadequate dialysis. Furthermore similar results have been reported from other centers in India (Rao et al. 1998). Studies from neighboring countries have also provided similar results – Nepal-17%[18] and Pakistan –31%.[19] In phase II of the study; monitoring of study group (group A) and thereafter enhancing dialysis length to maintain standardized Kt/V of two resulted in marked statistically significant improvement in clinical parameters, albumin and QoL. In our study mean arterial pressure fall in study group was 15.2 mm Hg as compared to 3.16 mm Hg in the control group which was statistically significant. Serum albumin has been traditionally considered as a marker of nutritional status in patients on regular hemodialysis. Serum albumin has a strong correlation with mortality in patients on hemodialysis.[20] However recent data suggests that it is also a marker of inflammation and chronic illness.[21] In our study, we found out that there was statistically significant rise in serum albumin in study group as compared to the control group. The average rise in serum albumin in study group was 0.47 g/dl as compared to 0.15 g/dl with P < 0.05. Anemia not only results in poor QoL in patients undergoing hemodialysis, but it is also a predictor of mortality. In our study, we found out that there was significant rise in Hb levels in patients of study group (1.47 g/dl) as compared to control group (0.15 g/dl) with P < 0.05 and Z score of 4.52. We found out that there was a significant improvement in WHO QoL score in study group (17.2) as compared to the control group (2.24) with P < 0.05 and Z score of 4.34. The improvement was largely seen in domains of - Physical and psychological. Other two domains – social and environmental remained unaffected.
The study also had several important limitations. Possibility of observer bias exists as blinding was not feasible. Also, this study has been done on a small sample size (n = 50) which limits the extrapolation to the general population. Hence randomized control study with a larger sample size would be required to confirm our findings. Exact residual kidney function was not assessed at the onset of the study. It plays a major contribution in total solute clearance, especially in removing middle, as well as small solute proteins.[22] One of RRF's major benefits is the optimization of fluid balance, blood pressure control, decreased left ventricular hypertrophy and reduction of cardiovascular disease. Also different variables such as drugs, transfusions, social circumstances, intermittent illness, nutrition, etc. were not analyzed. However, since both groups were randomized by computer generated randomization effect of these variables on study outcome was possibly minimal.
However increasing duration of hemodialysis even for few patients is not an easy task. The problem in increasing dialysis time and/or frequency is largely due to barriers to adoption of these alternative modalities rather than genuine disadvantages. The main barrier is the fact that no randomized controlled trial has yet demonstrated the clinical advantage of these strategies over conventional hemodialysis. Convincing patients to increase their session time and/or frequency is not easy, especially in India as patients often live far from dialysis centers and have to spend extra money from their meager economic resources. Patient education and financial support is crucial to bring about understanding and acceptance of prolonged or more frequent dialysis sessions.
In summary, Standard Kt/V can be used as an important tool to modify dialysis sessions to provide better QoL to the patients who are on twice per week hemodialysis. This tool is especially useful in India where patients live relatively far away from dialysis centers and have to spend considerable money to even travel to these centers. However, studies with larger sample size are required to conclusively prove our results.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Epidemiology and risk factors of chronic kidney disease in India – Results from the SEEK (screening and early evaluation of kidney disease) study. BMC Nephrol. 2013;14:114.
- [Google Scholar]
- International comparisons. United States Renal Data System. In: 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Vol Vol. 2. Atlas of ESRD; 2010.
- [Google Scholar]
- The global burden of chronic diseases: Overcoming impediments to prevention and control. JAMA. 2004;291:2616-22.
- [Google Scholar]
- Emperical prescription hemodialysis – Is there room for improvement. Indian J Nephrol. 1998;8:12-6.
- [Google Scholar]
- UK Renal Registry 13th Annual Report (December 2010): Chapter 8: Adequacy of haemodialysis in UK adult patients in 2009: National and centre-specific analyses. Nephron Clin Pract. 2011;119(Suppl 2):c141-7.
- [Google Scholar]
- US Renal Data System. USRDS 2005 Annual Data Report: Atlas of End-Stage Renal Disease in the United States, Bethesda, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases 2005
- Haemodialysis for end-stage renal disease in Southern India – A perspective from a tertiary referral care centre. Nephrol Dial Transplant. 1998;13:2494-500.
- [Google Scholar]
- NKF-DOQI clinical practice guidelines for hemodialysis adequacy. National Kidney Foundation. Am J Kidney Dis. 1997;30(3 Suppl 2):S15-66.
- [Google Scholar]
- Prevalence of the metabolic syndrome in an incident dialysis population. Hemodial Int. 2007;11:86-95.
- [Google Scholar]
- Functional status and quality of life: Predictors of early mortality among patients entering treatment for end stage renal disease. J Clin Epidemiol. 1991;44:83-9.
- [Google Scholar]
- NKF-K/DOQI Clinical Practice Guidelines for Hemodialysis Adequacy: Update 2000. Am J Kidney Dis. 2001;37(Suppl 1):S7-64.
- [Google Scholar]
- What do we know about chronic kidney disease in India:First report of the Indian CKD registry. BMC Nephrol. 2012;13:10.
- [Google Scholar]
- Regional variability in anaemia management and haemoglobin in the US. Nephrol Dial Transplant. 2003;18:147-52.
- [Google Scholar]
- Evaluation of dialysis adequacy in patients under hemodialysis and effectiveness of dialysers reuses. Nepal Med Coll J. 2009;11:107-10.
- [Google Scholar]
- Evaluation of nutritional status of patients on haemodialysis. J Coll Physicians Surg Pak. 2004;14:665-9.
- [Google Scholar]
- The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med. 1993;329:1001-6.
- [Google Scholar]
- Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol. 2010;21:223-30.
- [Google Scholar]
- Relative importance of residual renal function and convection in determining beta-2-microglobulin levels in high-flux haemodialysis and on-line haemodiafiltration. Blood Purif. 2007;25:295-302.
- [Google Scholar]







