Translate this page into:
Dobrin syndrome: A case report and review of the literature
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Dobrin syndrome or tubulointerstitial nephritis and uveitis syndrome is a rare disease with excellent prognosis. We report a 60-year-old male of Indian origin who presented with acute interstitial nephritis (AIN) and unilateral anterior immune-mediated uveitis. The syndrome has been reported sporadically. This is only the third case from a patient of Indian origin. We highlight this case and evaluate the long-term use of nonsteroidal anti-inflammatory drug-induced AIN and uveitis as a potential causative factor.
Keywords
NSAID
tubulointerstitial nephritis and uveitis syndrome
unilateral
Introduction
Dobrin syndrome, named after the US physician Robert S. Dobrin, (syn. tubulointerstitial nephritis and uveitis syndrome, TINU), was first described in 1975.[1] About 200 cases have been reported worldwide, including two each from India and Saudi Arabia.[23] People of Japanese, European, Hispanic, Asian and African descent are the most affected. In Japan, it is the second most frequently diagnosed disease in children with uveitis after sarcoidosis.[45] Cases have also been reported from the U.K.[46] A single case have been reported from Scandinavia, while many have been reported in Germany, where population has a similar genetic background to that of Scandinavians.[4]
This syndrome has two elements: acute idiopathic tubulointerstitial nephritis and uveitis, which can occur synchronously or metachronously.[6] The majority of patients are adolescents and young women.[78] There is a 3:1 female predominance. Long term ophthalmic and nephrology follow-up is essential to prevent organ damage.
Case Report
A 60-year-old male presented with blurred vision, redness, floaters and pain in the left eye. An ophthalmologist diagnosed a keyhole type pupil and anterior unilateral idiopathic uveitis. During follow-up and optical coherence tomography imaging [Figure 1], he was found to have unilateral cystoid macular edema and cotton wool spots. He was treated initially with left orbital floor injection of triamcinolone acetonide 10 mg/mL, topical dexamethasone OD for 4 weeks, and ketorolac tromethamine ophthalmic solution for 6 weeks. His vision improved considerably, but there was no improvement in the macular edema [Figure 1]. Another left orbital floor corticosteroid injection was given after 3 months, but with no improvement, after which he was commenced on high dose (1 mg/kg) of prednisolone for 4 weeks with a subsequent reducing regime over 3 months The patient was also on regular diclofenac 50/100 mg for severe knee pain for over 6 months, and calcium antagonist, esomoprozole and simvastatin.
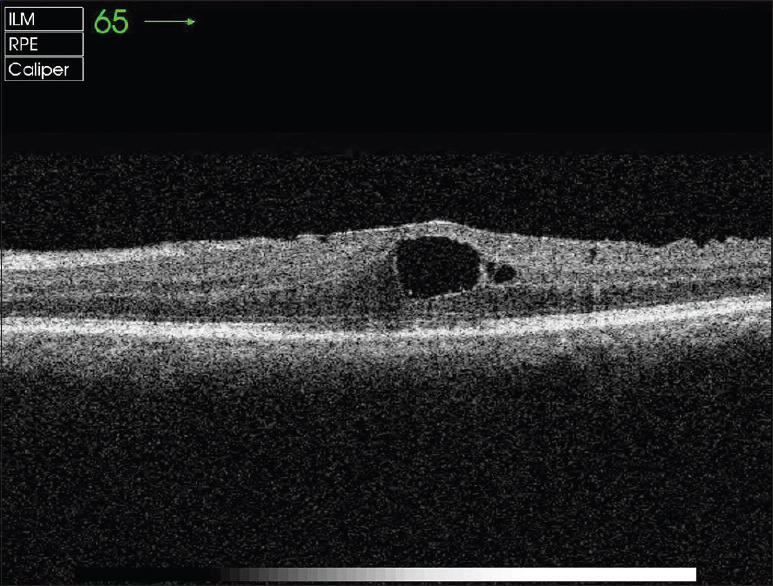
- Optical coherence tomography image shows left eye optic swelling and cystoid macular edema – active inflammation
Two weeks after starting on prednisolone, he complained of shivering, fever and sharp pain in the flank. Urine output fell, and serum creatinine rose. Laboratory assessment results are shown in Table 1. Renal ultrasound report showed normal sized kidneys. A kidney biopsy was performed, which showed tubulointerstitial nephritis, with no immune deposits. Oral prednisolone was continued, and diclofenac was withdrawn. There was an immediate and progressive improvement of the vision and renal function after the withdrawal of NSAID [Figure 2]. This was followed by complete resolution of the uveitis and kidney function. The renal function gradually returned to normal.


- Optical coherence tomography image shows no evidence of active inflammation in the left eye after the withdrawal of nonsteroidal anti-inflammatory drug
Discussion
The pathogenesis of Dobrin syndrome is not well understood. Limited evidence suggests that risk factors may include prior infection or drugs like antibiotics or NSAIDs.[9] Patients with uveitis usually present with bilateral and sometimes a unilateral alternating uveitis. Anterior uveitis is the predominant finding in the majority of cases, although a posterior uveitis can also be seen. It has been reported that uveitis occur before, concurrently, or up to 14 months after the onset of the interstitial nephritis. In majority of cases, uveitis usually presents after the silent onset of renal disease.[69]
It is estimated that in about 20% of patients with uveitis, intraocular complications like posterior synechiae, optic disc swelling, cystoids macular edema, chorioretinal scar formation, and later cataracts and glaucoma can develop.[7]
The diagnosis of Dobrin syndrome is suggestive of a combination of uveitis and renal involvement, with renal biopsy consistent with acute tubulointerstitial nephritis. There are no specific serum markers or laboratory findings that are unique to patients. Laboratory findings may include eosinophilia, anemia, slightly abnormal liver function tests, and an elevated erythrocyte sedimentation rate, renal insufficiency or sudden ARF, multiple proximal and distal tubular defects resulting in aminoaciduria, acidification defects, glucosuria and phosphaturia.[9]
The differential diagnosis may include sarcoidosis, tuberculosis, Sjögren's syndrome, systemic lupus erythematosus, Wegener's granulomatosis and Behçet's disease. Other differentials include ocular infections associated with tuberculosis, brucellosis, toxoplasmosis, glomerulonephritis, histoplasmosis, hyperthyroidism and drug-induced interstitial nephritis in a small percent of cases.[610]
The distinction of Dobrin syndrome from sarcoidosis and Sjögren's syndrome may also be challenging. In addition to uveitis and interstitial nephritis, Dobrin may also be associated with several systemic findings, including, fever, weight loss, fatigue, malaise, anorexia, arthralgia, myalgia, headache, polyuria, asthenia, abdominal and flank pain, and/or nocturia.[1112]
There have been no definitive identified familial, genetic or geographic clustering, but in a particular published study, some HLA-DQ antigenic determinants have been associated, namely with HLA-DQA1 × 01, HLA-DQB1 × 05 and HLA-DQB1 × 01 antigens; thus, increasing the possibility of genetic risk factors.[13]
Patients with progressive renal insufficiency are typically treated with prednisone at a dose of 1 mg/kg/day for 3 to 6 months and then slowly tapered. Majority of the patients recover absolute normal renal function and sight. This regimen is similar to (but more prolonged) therapy for AIN. However, relapses are more likely to occur in Dobrin syndrome because of the potential immunologic basis of the disease.[611]
The acute tubulointerstitial nephritis in this case could be related to the NSAID use as well, since the condition resolved following withdrawal of the agent.
Conclusion
The renal disease in Dobrin syndrome seems to have an excellent prognosis, with complete resolution if treated early with selective corticosteroid therapy. A multidisciplinary approach is crucial for the prompt recognition, effective management and control of the disease activity and for drug regimen optimization.
Acknowledgment
The authors would like to acknowledge Drs. Razique Anwer and Mohammad Fareed for their valuable help in this mauscript and Mr. Shahee, of the London Moorfield Eye Hospital, UK for OCT Imaging.
Source of Support: The work was not supported or funded by any source
Conflict of Interest: The authors have no conflict of interests.
References
- Acute eosinophilic interstitial nephritis and renal failure with bone marrow-lymph node granulomas and anterior uveitis. A new syndrome. Am J Med. 1975;59:325-33.
- [Google Scholar]
- Tubulointerstitial nephritis with uveitis syndrome: A case report and review of literature. Indian J Nephrol. 2010;20:103-5.
- [Google Scholar]
- Acute tubulointerstitial nephritis and anterior uveitis (TINU syndrome): A report of two cases. Saudi J Kidney Dis Transpl. 2006;17:386-9.
- [Google Scholar]
- Tubulointerstitial nephritis and uveitis (TINU) syndrome: A case report and review of the literature. Acta Ophthalmol. 2009;87:676-9.
- [Google Scholar]
- Acute renal failure due to idiopathic tubulo-intestinal nephritis and uveitis: “TINU syndrome”. Case report and review of the literature. J Nephrol. 2000;13:377-80.
- [Google Scholar]
- Tubulointerstitial nephritis and uveitis (TINU syndrome). Topic in UpToDate (Ministry of Health). Wolters Kluwer publication 2014; Topic 7189, Version 10.0.
- [Google Scholar]
- Tubulointerstitial nephritis and uveitis syndrome in a twelve-year-old girl. Case Rep Pediatr 2013 2013:652043.
- [Google Scholar]
- A case of tubulointerstitial nephritis and uveitis syndrome in an elderly patient. Korean J Ophthalmol. 2012;26:398-401.
- [Google Scholar]
- The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol. 2001;46:195-208.
- [Google Scholar]
- Hyperthyroidism: A novel feature of the tubulointerstitial nephritis and uveitis syndrome. Pediatrics. 1999;104:314-7.
- [Google Scholar]
- Acute interstitial nephritis and uveitis syndrome: Activated immune cell infiltration in the kidney. Pediatr Nephrol. 1991;5:232-4.
- [Google Scholar]
- Course and outcome of tubulointerstitial nephritis and uveitis syndrome. Am J Kidney Dis. 1999;34:1016-21.
- [Google Scholar]
- Strong associations between specific HLA-DQ and HLA-DR alleles and the tubulointerstitial nephritis and uveitis syndrome. Invest Ophthalmol Vis Sci. 2003;44:653-7.
- [Google Scholar]







