Translate this page into:
Effect of inflammation on nutritional status of patients on maintenance hemodialysis
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Malnutrition is a major hurdle for long time survival in patients on maintenance hemodialysis (MHD).[1] We evaluated the effect of inflammation on nutritional status in 90 patients (56 males; age 52.6 ± 11.7 years) on MHD for >6 months. Seventy healthy controls (35 males; age 50.6 ± 9.7 years) were also studied. Demographics and dialysis-related data including duration of dialysis and dialysis adequacy for cases were collected. Serum inflammatory markers tumor necrosis factor alpha (TNF-α) by ELISA and high-sensitivity C-reactive protein (hs-CRP) by immunoturbidimetry were assessed for cases and controls. Nutritional status was assessed using subjective global assessment-dialysis malnutrition score (SGA-DMS).[2] A score of 7–10 was considered as well nourished, 11–20 as mild to moderately malnourished, and 21–35 as moderate to severely malnourished.
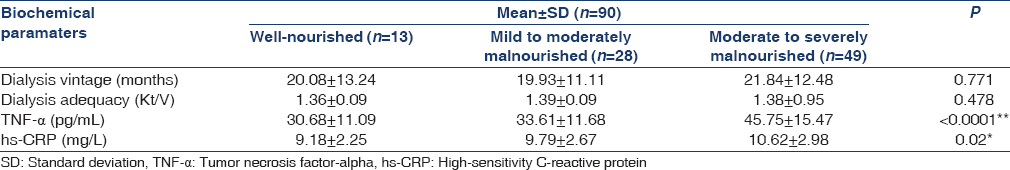
The mean dialysis vintage was 20.99 ± 12.08 months and the mean Kt/V was 1.38 ± 0.09. Of 90 cases, 14.4% were well nourished, whereas 31% showed mild to moderate and 54.4% moderate to severe malnutrition. The mean serum TNF-α (39.798 ± 15.19 vs. 6.539 ± 1.22 pg/ml) and hs-CRP (10.158 ± 2.82 vs. 2.66 ± 0.535 mg/L) were elevated in hemodialysis patients compared to control (P < 0.0001). There was no difference in the duration of dialysis and dialysis adequacy based on the nutritional status. There was a difference in the TNF-α (P < 0.0001) and hs-CRP levels (P = 0.02) with respect to the nutritional status. A positive correlation was observed between TNF-α and SGA-DMS (r = 0.630; P < 0.0001) and hs-CRP and SGA-DMS (r = 0.381; P < 0.0001) indicating an increase in the levels of inflammatory markers with an increase in the SGA-DMS scores, which reflected a decline in the nutritional status [Table 1].
In Indian population, there is a 50–65% prevalence of mild to severe malnutrition amongst patients with ESRD. Compared to the Western world, the prevalence is higher in Indian patients which could be possibly due to poor socioeconomic status and related consequences like inability to afford to adequate renal nutrition.[34] The prevalence of inflammation varies from 30% to 75% in chronic kidney disease patients and the reasons include factors related to uremia such as decreased clearance of cytokines, oxidative stress, accumulation of advanced glycation end products, and infectious complications and dialysis-related factors such as membrane bioincompatibility, vascular access infections, and endotoxin exposure that stimulates the inflammatory response by activating the production of inflammatory cytokines.
TNF-α, produced by activated macrophage monocytes, plays an important role in the pathogenesis of inflammation and is strongly associated with malnutrition. It is also evident that TNF-α is a more precise marker for predicting nutritional and inflammatory status than hs-CRP.[5]
Patients on MHD suffer an inflammatory state which is strongly associated to malnutrition and anorexia. Therapeutic interventions to decrease inflammation are the need of the hour to alleviate malnutrition-inflammation syndrome in patients on MHD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Malnutrition-inflammation complex syndrome in dialysis patients: Causes and consequences. Am J Kidney Dis. 2003;42:864-81.
- [Google Scholar]
- A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant. 1999;14:1732-8.
- [Google Scholar]
- High prevalence of malnutrition and inflammation in undialyzed patients with chronic renal failure in developing countries: A single center experience from eastern India. Ren Fail. 2007;29:811-6.
- [Google Scholar]
- Nutritional status of patients undergoing maintenance hemodialysis. J Community Nutr Health. 2013;2:38-47.
- [Google Scholar]
- Inflammation in end-stage renal disease: Sources, consequences, and therapy. Semin Dial. 2002;15:329-37.
- [Google Scholar]






