Translate this page into:
N-acetyl cysteine versus allopurinol in the prevention of contrast nephropathy in patients with chronic kidney disease: A randomized controlled trial
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Contrast media administration can lead to acute deterioration in renal function particularly in patients with pre-existing chronic kidney disease. This prospective, randomized controlled open-label parallel group study was undertaken at Nizam's Institute of Medical Sciences, Hyderabad, from June to December 2015. A total of 95 patients were included, of which 35 received n-acetylcysteine (NAC) + normal saline (NS), 30 patients received allopurinol (ALL) + NS, and 30 patients received placebo. In our study, the overall incidence of CIN was 24%. Incidence of CIN in NAC + NS, ALL + NS, and placebo group were 20%, 16%, and 36%, respectively. The major finding of this study was there was no significant difference between NAC and allopurinol in the prevention of contrast nephropathy. However, only allopurinol was superior to placebo. In our study, hyperuricemia and baseline serum creatinine were the only risk factors associated with CIN.
Keywords
Allopurinol
chronic kidney disease
contrast nephropathy
N-acetylcysteine
Introduction
Contrast-enhanced imaging services have been widely used over the past decade. Contrast media can lead to acute deterioration in renal function particularly in patients with pre-existing chronic kidney disease. About 12–14% of patients who develop acute renal sufficiency during hospitalization do so after procedures involving radiographic contrast.[12] The incidence of progressive deterioration can be as high as 42% in patients with abnormal baseline renal function.[34]
Several protocols have been tested for the prevention of radiocontrast-induced acute kidney injury including periprocedural hydration with isotonic or hypotonic saline, antioxidant compounds such as N-acetyl cysteine (NAC), ascorbic acid[5] or allopurinol and the use of low or iso–osmolar contrast agents, hemofiltration,[6] or dialysis.[7] Conflicting evidence suggests that administration of NAC prevents this renal impairment. Few studies[8] have shown that prophylactic oral administration of allopurinol, along with hydration, may protect against contrast-induced nephropathy (CIN) in high-risk patients undergoing coronary procedures. Very few studies[9] compared NAC and allopurinol in the prevention of CIN. The results were disappointing or inconclusive and intravenous volume expansion remains to date the only measure of undisputed efficacy.
This study compared the efficacy of NAC versus allopurinol in addition to intravenous hydration with normal saline (NS) as prophylaxis for CIN in patients with impaired renal function undergoing planned coronary angiography or intervention.
Materials and Methods
This prospective, randomized controlled open-label parallel group study was undertaken at Nizam's Institute of Medical Sciences, Hyderabad, from June 2015 to December 2015.
Patients undergoing clinically driven nonemergent coronary angiography and percutaneous coronary interventions for both stable and unstable patients with angina, non-ST-segment elevation myocardial infarction (NSTEMI) and acute myocardial infarction/STEMI were included in this study. They are as follows:
-
Age more than 30 years
-
Patients should have their serum creatinine ≥1.2 mg/dl on their most recent sample drawn within 3 months of planned procedure.
Patients with acute renal failure, endstage renal disease requiring dialysis, intravascular administration of contrast material within previous 6 days, pregnancy, lactation, emergent coronary angiography, history of hypersensitivity reaction to contrast media, cardiogenic shock, pulmonary edema, mechanical ventilator, parenteral use of diuretics, recent use of NAC, recent use of ascorbic acid, and use of metformin or NSAIDS within 48 h of procedure were excluded from the study.
All eligible patients were divided into three groups. They are as follows:
-
NAC + NS: Group of patients who received NS and NAC
-
ALL + NS: Group of patients who received NS and allopurinol
-
Placebo + NS: Group of patients who received NS only
A total of 95 adult patients of age >30 years with serum creatinine ≥1.2 undergoing IV contrast study for coronary angiography or interventions were enrolled in this study. Quantity of IV contrast given to all patients was recorded along with baseline and post procedure serum creatinine. All patients received IV iodixanol. All the details of patients such as age, gender, and comorbidities (presence of hypertension [HTN], diabetes, and coronary artery disease) were noted. Uric acid levels were measured in all patients prior, and allopurinol was given irrespective of uric acid level. Phases of the study are shown in Figure 1.
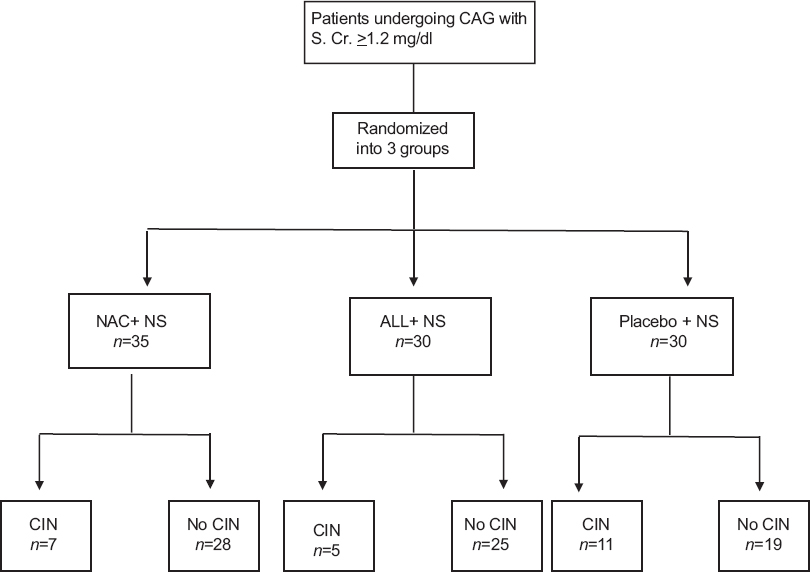
- Flow diagram of the phases of the study. NAC: N-Acetyl cysteine, NS: Normal saline, ALL: Allopurinol, CIN: Contrast-induced nephropathy
Serum creatinine, blood urea, electrolytes were done before and every 24 h for 2 days after the study. The effect of modality was evaluated by observing the change in serum creatinine from baseline.
Isotonic normal saline was infused at a rate of 0.5 ml/kg/h 12 h prior to the procedure and was continued for 12 h after contrast administration (total 24 h). Those patients who had low ejection fraction (<40%) received NS at rate of 0.3 ml/kg/h. NAC was given 600 mg orally twice daily, the day before and the day of the procedure. single oral dose of 300 mg of allopurinol was given the day before the procedure. CIN, defined as either a relative increase in serum creatinine from baseline of ≥25% or an absolute increase of ≥0.3 mg/dl (44.2 µmol/L) during days 1 and 2.
A total of 95 patients were enrolled into the study with confidence level of 95% and power of 80% to determine the significant change between treatment groups. This study was planned as randomized pilot study in which the sample size calculation was based on standard measures of confidence levels and power, based on previous studies involving the study drugs. No effect sizes were assumed.
Statistical analysis
Data were presented as mean ± standard deviation. Descriptive statistics were applied for the entire sample and for the treatment subgroups. Odds ratio analysis was performed between the treatment groups to determine the association. Odds ratio was calculated using MedCalc for Windows, Version 16.4.3 (MedCalc Software, Ostend, Belgium). P < 0.05 was considered to be significant.
Results
The baseline characteristics in the study groups are shown in Table 1. As shown in Table 2, there was no significant difference between NAC and allopurinol in the prevention of contrast nephropathy. However, when compared with placebo alone only allopurinol was proved to be superior. As shown in Tables 3 and 4, odds ratio for age-CIN was 1.07, indicating an association between age >60 years and the development of CIN. However, this was not determined to be statistically significant (P > 0.05), and a similar association between age >60 years and development of CIN was observed in ALL + NS group, without statistical significance. The odds ratio for gender-CIN was 1.2, indicating an association between male sex and the development of CIN. However, this was not determined to be statistically significant (P > 0.05); on analysis of the treatment groups, a similar association between male sex and development of CIN was observed in ALL + NS group and NAC + NS group, however without statistical significance. The odds ratio for DM-CIN was 0.62, indicating no association between DM and the development of CIN; on analysis of the treatment groups, an association between DM and development of CIN was observed in ALL + NS group, however without statistical significance. The odds ratio for HTN-CIN was 1.14, indicating an association between HTN and the development of CIN; however, this was not determined to be statistically significant (P > 0.05); on analysis of the treatment groups, a similar association between HTN and development of CIN was observed in ALL + NS group without statistical significance.




The odds ratio for preprocedural SBP-CIN was 0.77, indicating no association between preprocedural SBP and the development of CIN; on analysis of the treatment groups, an association between preprocedural SBP and development of CIN was observed in ALL + NS group and NAC + NS without statistical significance. The odds ratio for preprocedural DBP-CIN was 0.88, indicating no association between preprocedural DBP and the development of CIN; on analysis of the treatment groups, no association was observed between preprocedural DBP and development of CIN. The odds ratio for contrast volume-CIN was 0.8, indicating no association between contrast volume and the development of CIN; on analysis of the treatment groups, no association between contrast volume and development of CIN was observed in all three groups.
The odds ratio for anemia-CIN was 1.8, indicating an association between anemia and the development of CIN. However, this was not determined to be statistically significant (P > 0.05). On analysis of the treatment groups, an association between anemia and development of CIN was observed in placebo group, however without statistical significance. The odds ratio for uric acid-CIN was 2.3, indicating an association between uric acid and the development of CIN and it was not statistically significant (P > 0.05). Incidence of CIN in hyperuricemia group was 35% and 19% in normouricemic group. Upon odds ratio analysis of the treatment groups, an association between uric acid and development of CIN was observed in ALL + NS group and placebo, however without statistical significance in ALL + NS group and it was statistically significant in the NS group. The odds ratio for albumin-CIN was 0.91, indicating no association between albumin and the development of CIN; on analysis of the treatment groups, no association between albumin and development of CIN was observed in all three groups. Analysis shows that an association was found between baseline serum creatinine and CIN, which was statistically significant; upon odds ratio analysis of the treatment groups, an association between baseline serum creatinine and development of CIN was observed in all three groups without statistical significance.
Overall six patients needed dialysis; one patient in NAC group, one patient in allopurinol group, and four in placebo group. Four patients improved after few sessions of hemodialysis, two patients became dialysis dependent in placebo group. One patient died of sudden cardiac arrest before giving dialysis support in allopurinol group.
Discussion
The main objective of this study was to compare NAC and allopurinol in the prevention of contrast nephropathy in patients with impaired renal function. The major finding of this study was absence of difference between NAC and allopurinol in the prevention of contrast nephropathy. However, compared with placebo alone only allopurinol was superior.
In our study, the overall incidence of CIN was 24%. Incidence of CIN in NAC + NS, ALL + NS, and placebo group were 20%, 16%, and 36%, respectively.
To the best of our knowledge, this is the first study comparing NAC and allopurinol in the prevention of CIN in patients with pre-existing CKD. A similar study was done by Kumar et al.[9] in 2014 comparing NAC and allopurinol in the prevention of contrast nephropathy in patients undergoing cardiac catheterization with normal baseline serum creatinine and showed that prophylactic administration of allopurinol along with hydration was better than NAC and hydration for protection against CIN. They showed that in patients receiving iodixanol as contrast agent, the incidence of CIN in allopurinol and hydration were 0% and 30%, respectively.
Erol et al.[8] analyzed efficacy of allopurinol pretreatment for the prevention of CIN. In this study, 159 patients were enrolled with baseline serum creatine >1.1 mg/dl. Patients were randomized to either allopurinol + NS or hydration alone. Mean serum creatine was around 1.45 mg/dl. CIN occurred in 7.5% of patients in hydration alone group and 0% in allopurinol group. Erol et al.[8] concluded that allopurinol along hydration may protect against CIN in high-risk patients undergoing coronary procedures.
Our study also showed similar results such that allopurinol along with hydration was superior to hydration alone in the prevention of CIN. In our study, incidence of CIN in allopurinol group was 16% compared to 36% in hydration group alone, which was statistically significant. As shown in Table 5 incidence of CIN was high both in allopurinol and hydration group in our study when compared to studies done by Erol et al.[8] and Kumar et al.[9] probably due to high baseline creatinine and increase of >0.3 mg/dl being taken as CIN.

In our study, the incidence of CIN in NAC + NS subgroup was 20%, and in hydration only group was 36%. Our study showed that NAC + NS was superior to hydration alone in the prevention of CIN, although statistically not significant. Several studies compared hydration with NS, with or without NAC in the prevention of CIN in patients with elevated renal parameters.
Table 6 compare various studies regarding NAC in the prevention of CIN. Ramesh et al.[10] in 2006 compared NAC with hydration in the prevention of contrast nephropathy in patients with elevated serum creatine (≥1.5 mg/dl). The incidence of CIN in NAC + NS and hydration alone groups was 4% and 29%, respectively. This study showed that NAC was superior to hydration alone which was statistically significant.

Tepel et al.[11] prospectively studied 83 patients with chronic renal insufficiency with mean serum creatinine 2.4 ± 1.3 mg/dl. Patients were randomly assigned to receive either NAC and 0.45% NS or placebo with saline. Incidence of CIN in NAC + NS group was 2%, 21% placebo and saline group, which were statistically significant.
Calabrò et al.[12] showed that intravenous hydration with saline and NAC is an effective and low-cost tool in preventing CIN in patients undergoing coronary artery angiography. Marenzi et al.[13] showed that intravenous and oral NAC may prevent contrast nephropathy with a dose-dependent effect.
Durham et al.[14] conducted a randomized controlled trial of NAC to prevent contrast nephropathy in cardiac angiography. Patients were recruited with serum creatinine >1.7 mg/dl. Total of 79 patients were enrolled in the study. CIN developed in 26.3% of NAC group and 22% of placebo group (hydration alone). This study shows that NAC was not effective for the prevention of CIN after cardiac angiography (P = 0.09).
Allaqaband et al.[15] showed that in patients with chronic renal insufficiency, NAC or fenoldopam offered no additional benefit over hydration with saline in preventing CIN.
In our study, uric acid and baseline serum creatinine were the only risk factors associated with CIN. Age, male sex, history of hypertension, hemoglobin <12 g/dl, diabetes mellitus, preprocedural systolic and diastolic blood pressure (SBP and DBP), volume of contrast and serum albumin were were not significantly associated with CIN.
Toprak et al.[16] assessed hyperuricemia as a risk factor for CIN in patients with chronic kidney disease. CIN occurred in 15.1% of hyperuricemic group and 2.9% of the normouricemic group (P < 0.001); Hypoalbuminemia and age >70 years were other risk indicators. In our study, the incidence of CIN in hyperuricemia group was 35% and 19% in normouricemic group. CIN incidence was high in our study due to high baseline serum creatinine and >0.3 mg/dl increase being taken as CIN.
Toprak et al.[17] in 2006 showed that patients with diabetes are at high risk of developing CIN. CIN occurred in 20% of the DM patients and 11.4% of the pre-DM, and 5.5% of normal group. In our study, 20% of DM patients develop CIN, similar to Toprak et al. but there was no statistical difference between diabetics and nondiabetics developing CIN may be due to other risk factors influencing CIN.
McCullough et al.[1] showed that the risk of CIN is minimal in patients receiving <100 ml contrast volume. Klein et al.[18] showed that in the diabetic population, CIN developed every fifth, fourth, and second patient who received 200–400, 400–600, >600 ml contrast study, respectively. In our study, no significant association was found between patients who received contrast volume >100 ml and CIN. The probable reason could be the mean contrast volume used in our study was low, around 70 ml.
This single-center study had small number of cases. Rise in serum creatinine was observed only for 48 h. In some patients, there could have been late rise in serum creatinine which were probably missed. The type of acute renal failure (ischemic, nephrotoxic, or atheroembolic) could not be determined precisely as renal biopsies were not performed. Because of the nature of the patients and the procedures being performed, acute rise in serum creatinine was assumed to be multifactorial.
Conclusions
We concluded that there was no significant difference between NAC and allopurinol in the prevention of contrast nephropathy in patients with impaired renal function. Allopurinol along with hydration was better than hydration alone in the prevention of CIN. Overall incidence of CIN was high. Hyperuricemia and baseline serum creatinine were the only risk factors associated with CIN.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acute renal failure after coronary intervention: Incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368-75.
- [Google Scholar]
- Hospital-acquired renal insufficiency: A prospective study. Am J Med. 1983;74:243-8.
- [Google Scholar]
- Risks for renal dysfunction with cardiac angiography. Ann Intern Med. 1986;104:501-4.
- [Google Scholar]
- Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med. 1989;86(6 Pt 1):649-52.
- [Google Scholar]
- Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation. 2004;110:2837-42.
- [Google Scholar]
- The prevention of radiocontrast-agent-induced nephropathy by hemofiltration. N Engl J Med. 2003;349:1333-40.
- [Google Scholar]
- Extracorporeal blood purification therapies for prevention of radiocontrast-induced nephropathy: A systematic review. Am J Kidney Dis. 2006;48:361-71.
- [Google Scholar]
- Efficacy of allopurinol pretreatment for prevention of contrast-induced nephropathy: A randomized controlled trial. Int J Cardiol. 2013;167:1396-9.
- [Google Scholar]
- Comparative study of renal protective effects of allopurinol and N-acetyl-cysteine on contrast induced nephropathy in patients undergoing cardiac catheterization. J Clin Diagn Res. 2014;8:HC03-7.
- [Google Scholar]
- Reno-protective effect of N-acetyl cysteine in patients with impaired renal function undergoing coronary angiography and interventions. J Assoc Physicians India. 2006;54:449-52.
- [Google Scholar]
- Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000;343:180-4.
- [Google Scholar]
- Use and efficacy of saline hydration and N-acetyl cysteine to prevent contrast-induced nephropathy in low-risk populations undergoing coronary artery angiography. Intern Emerg Med. 2011;6:503-7.
- [Google Scholar]
- N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006;354:2773-82.
- [Google Scholar]
- A randomized controlled trial of N-acetylcysteine to prevent contrast nephropathy in cardiac angiography. Kidney Int. 2002;62:2202-7.
- [Google Scholar]
- Prospective randomized study of N-acetylcysteine, fenoldopam, and saline for prevention of radiocontrast-induced nephropathy. Catheter Cardiovasc Interv. 2002;57:279-83.
- [Google Scholar]
- Hyperuricemia as a risk factor for contrast-induced nephropathy in patients with chronic kidney disease. Catheter Cardiovasc Interv. 2006;67:227-35.
- [Google Scholar]
- Impact of diabetic and pre-diabetic state on development of contrast-induced nephropathy in patients with chronic kidney disease. Nephrol Dial Transplant. 2007;22:819-26.
- [Google Scholar]
- The use of radiographic contrast media during PCI: A focused review: A position statement of the Society of Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2009;74:728-46.
- [Google Scholar]







