Translate this page into:
A Study of Clinical Presentation and Correlative Histopathological Patterns in Renal Parenchymal Disease
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Suspicion and subsequent detection of renal disease is by an assessment of the urinalysis and renal function in the clinical context. Our attempt in this study is to correlate initial presenting features of urinalysis and renal function to the final histopathological diagnosis. A retrospective analysis of 1059 native kidney biopsies performed from January 2002 to June 2015 at Amrita Institute of Medical Sciences was conducted. Correlative patterns between urinalysis, renal function, and final histopathological diagnosis were studied. Five hundred and eleven (48%) patients had nephrotic syndrome. Out of these, 193 (38%) had pure: nephrotic syndrome, 181 (35.8%) had associated microhematuria, 110 (21.7%) had microhematuria and renal failure, and 27 (5.3%) had only associated renal failure. Minimal change disease (MCD) (30%), membranous nephropathy (30%), and IgA nephropathy (29%) were the major diseases in the respective groups. Five hundred and five (47.6%) patients had subnephrotic proteinuria. Out of these, 29 (5.6%) had only subnephrotic proteinuria, 134 (27%) had additional microhematuria, 300 (59%) had subnephrotic proteinuria, microhematuria, and renal failure, and 42 (8%) had subnephrotic proteinuria with renal failure. Lupus Nephritis (45% and 40%) and IgA Nephropathy (32% and 21%) were the major disorders in the subgroups respectively. Forty-two patients (3.7%) were biopsied for isolated renal failure with bland urinary sediment. Cast nephropathy and acute interstitial nephritis were the major diseases. Out of 89 patients with diabetes who were biopsied, 15 (16.8%) had diabetic nephropathy, 45 (50.5%) had no diabetic nephropathy, and 29 (32.5%) had diabetic nephropathy along with a non-diabetic renal disease. Postinfectious glomerulonephritis was the major glomerular disease. IgA nephropathy (22.2%) and membranous nephropathy (15.5%) were the major diseases in patients with diabetes with no diabetic nephropathy. In our population, MCD and membranous nephropathy formed the majority of diseases in biopsied nephrotic syndrome. Added microhematuria did not seem to decrease the incidence of either disease on the whole. We found a significant number of patients with membranous nephropathy with nephrotic syndrome, microhematuria, and additional renal failure. IgA nephropathy formed a majority of cases with nephrotic syndrome, microhematuria, and renal failure. The presence of renal failure regardless of other abnormalities in urinalysis showed a trend toward IgA nephropathy. Membranous nephropathy may have a more varied presentation than was originally thought and IgA nephropathy presenting as nephrotic syndrome may not be uncommon. MCD is the major subgroup of diseases in the pediatric population and presents both as nephrotic syndrome as well as nephrotic syndrome with microhematuria. Thus, urinalysis and renal failure may be a valuable tool in assessing renal disease.
Keywords
Clinicopathological correlation
histopathology
renal failure
urinalysis
Introduction
Percutaneous renal biopsy is the mainstay of diagnosis of renal parenchymal disease. General indications of renal biopsy are significant proteinuria (>1 g/day or equivalent spot protein/creatinine ratio), microscopic hematuria with any degree of proteinuria, unexplained renal impairment (native or transplanted kidney), and renal manifestations of systemic disease.
Often, suspicion and subsequent detection of renal disease is by an assessment of the urinalysis, mainly proteinuria and microhematuria along with severity of renal failure in varying combinations, in the appropriate clinical context. Although there are established patterns of presentation for most diseases, variations in presentation occur based on the geographic area, age, sex, and socioeconomic conditions. Our attempt in this study is to correlate initial presenting features of urinalysis and renal failure to the final histopathological diagnosis.
Methods
A retrospective analysis of 1059 native kidney biopsies performed from January 2002 to June 2015 at Amrita Institute of Medical Sciences was conducted. Correlative patterns between urinalysis, renal failure, and final histopathological diagnosis were studied. Desired ethical clearance was obtained for the same. We defined nephrotic proteinuria as urine protein more than 3.5 grams/day, Subnephrotic proteinuria as urine protein less than 3.5 grams/day, microhematuria as more than 3 RBCs per high power field and renal failure as S. Creatinine more than 1.4 mg/dl.
Results
1059 native kidney biopsies were analyzed. The general trend of renal biopsies at our Institute is as follows: 229 IgA nephropathy (21.6%), 105 membranous nephropathy (10%), 118 lupus nephritis (11.1), 93 minimal change disease (MCD) (8.7%), and 85 focal segmental glomerulosclerosis (FSGS) (8%). Mean age of our study population was 38 years. 55.4% (587) were males and 44.6% (472) were female.
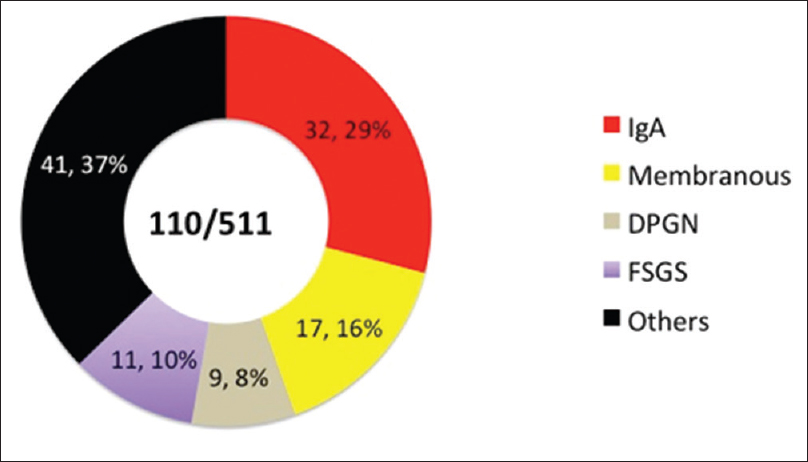
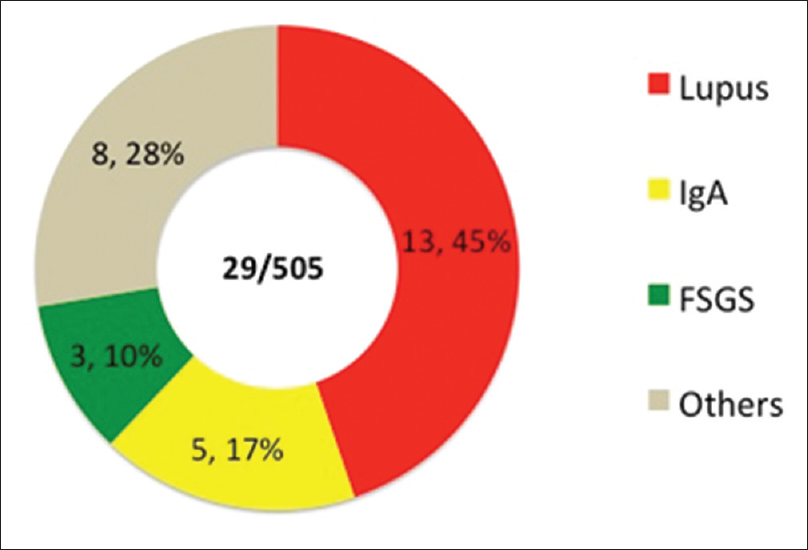
We divided our patients into two main cohorts: nephrotic and subnephrotic proteinuria. Each cohort was further subdivided into additional groups with microhematuria and renal failure, and the disease distribution was studied. For the purpose of discussion, we have categorized these groups as: (I) Nephrotic syndrome, (II) Nephrotic syndrome with microhematuria, (III) Nephrotic syndrome with microhematuria and renal failure, (IV) Subnephrotic proteinuria with microhematuria, (V) Subnephrotic proteinuria with microhematuria and renal failure, (VI) pure subnephrotic proteinuria, and (VII) Subnephrotic proteinuria and renal failure. Group I had MCD (30%) followed by IgM nephropathy (19%) [Figure 1]. FSGS comprised 14% of this group. Nearly 16% of pure nephrotic syndromes were proven membranous nephropathy. In Group II and III, membranous nephropathy formed 30% and 16% of the cases, respectively [Figures 2 and 3]. In Group II, membranous nephropathy comprised the major subgroup (30%) followed by MCD (18%), FSGS (16%) and IgA Nephropathy. In Group III, IgA nephropathy formed the major subgroup of diseases (29%), followed by membranous nephropathy (16%), FSGS (10%), and postinfectious glomerulonephritis (8%) [Figure 3]. Group IV was comprised of lupus nephritis (40%) and IgA nephropathy (34%) [Figure 4]. IgA nephropathy was the major disease in Group V (32%) [Figure 5], lupus nephritis comprised 45% of patients in Group VI [Figure 6], and IgA nephropathy (21.4%) in Group VII [Figure 7]. Sixty-nine patients with combinations of renal failure and proteinuria were biopsied. The results are depicted in Figure 7. IgA nephropathy formed the majority of patients in this group. It was further subdivided into nephrotic and subnephrotic proteinuria. A minor subgroup (42) of patients was biopsied for unexplained renal failure without any abnormality in urinalysis. Cast nephropathy (23.8%) and acute interstitial nephritis (21.4%) were the major diseases in this group. Results have been summarized in Figures 8–9 and Table 1.

- Group I: Nephrotic syndrome

- Group II: Nephrotic proteinuria + microhematuria
- Group III: Nephrotic proteinuria + microhematuria + renal failure

- Subnephrotic proteinuria + microhematuria

- Subnephrotic proteinuria + microhematuria + renal failure
- Subnephrotic proteinuria

- Renal failure + proteinuria

- Nephrotic proteinuria: Summary

- Subnephrotic proteinuria: Summary

Eighty-nine patients with type 2 diabetes mellitus were biopsied for various indications. Fifteen (16.8%) patients had pure diabetic nephropathy, 45 (50.5%) had no diabetic nephropathy, and 29 (32.5%) had diabetic nephropathy along with a nondiabetic disease. Postinfectious glomerulonephritis was the major glomerular disease in the latter group [Figure 10]. IgA nephropathy (22.2%) and membranous nephropathy (15.5%) were the major diseases in patients with diabetes with no diabetic nephropathy [Figures 10 and 11].

- Biopsy-proven diabetic nephropathy + nondiabetic renal disease

- Nondiabetic renal disease without diabetic nephropathy
One hundred and sixty-four biopsies (15.4%) were in the pediatric population (<18 years). The trend of renal biopsies was: 38 MCD (23.1%), 32 lupus nephritis (19.5%), 22 IgM nephropathy (13.4%), 10 IgA nephropathy (6%), 9 FSGS (5.4%), and 4 (2.4%) postinfectious glomerulonephritis. The mean age of children biopsied was 11 years, and 57% (93) were males and 43% (70) were females. After dividing pediatric biopsies into similar groups as done for adults, Group I (pure nephrotic syndrome) formed the major subgroup of pediatric bipsies (43.2%). Main diseases in this group were MCD (39%) and IgM nephropathy (29.5%). Group II (19.5% of pediatric biopsies) was comprised MCD (28%) and lupus nephritis (21.8%). Groups IV and V formed 17% and 9% of pediatric biopsies, respectively, and both groups showed lupus nephritis as the major component (57% and 33.3%, respectively).
Discussion
The prevalence of biopsy-proven renal disease varies according to geographic areas, socioeconomic conditions, race, age, and indications for renal biopsy. The onset of many renal diseases is “silent,” and the diagnosis is sometimes made by urine testing during a routine medical examination. Previous analysis of native kidney biopsies in India has been made at Christian Medical College, Vellore.[1] Our attempt was to analyze the spectrum of renal disease in Kerala and also to correlate final biopsy diagnosis with the presenting urinalysis and renal failure.
Nephrotic syndrome may occur with a variety of primary and systemic diseases. MCD is the dominant cause in children. In adults, approximately 30% have a systemic disease such as amyloidosis, or systemic lupus erythematosus; the remaining are due to primary renal disorders such as MCD, FSGS, and membranous nephropathy[23456789] Previous studies have shown that up to 50% of cases of membranous nephropathy may have microhematuria.[10] In Group II, membranous nephropathy comprised the major subgroup (30%) as opposed to our expectation of IgA nephropathy (10%) or FSGS (16%) [Figure 4]. MCD formed the next major group of diseases in this group (18%). Microhematuria has been described in up to 29% of adult MCD.[11] Thus, the classical incidence of causes of nephrotic syndrome, i.e. MCD and membranous nephropathy was not significantly altered statistically with the inclusion of microhematuria. In Group III, however, IgA nephropathy formed the major subgroup of diseases (29%), interestingly followed by membranous nephropathy (16%), FSGS (10%), and postinfectious glomerulonephritis (8%) [Figure 3]. This is at odds with classical descriptions of IgA nephropathy presentation, where only 10% of IgA nephropathy cases present as nephrotic syndrome with varying degrees of proteinuria and renal failure.
Group IV was dominated by lupus nephritis (40%) and IgA nephropathy (34%) [Figure 7]. Previous studies in India have shown a preponderance of Class IV and Class II lesions,[12] with which our reports are also in agreement with 48% being ISN/RPS Class IV and 35% being Class III. The proliferative pathology associated with these classes explains the predominance of lupus in this group. In our database, we had an almost equal percentage of IgA nephropathy in Group III (29%), Group IV (34%), and Group V (32%) although the absolute number of cases was much more in the latter (97). These results are at par with other studies with 30%–40% of IgA nephropathy cases presenting with subnephrotic proteinuria and microhematuria.[1314]
Thus, urine sediment and histopathological correlation is useful in predicting the possibility of a disease process. MCD and membranous nephropathy formed the majority of diseases in biopsied pure nephrotic syndrome (62%). The presence of added microhematuria did not seem to decrease the incidence of either disease on the whole. We found a significant number of patients with membranous nephropathy with nephrotic syndrome, microhematuria, and additional renal failure (16%). IgA nephropathy formed a majority of cases with subnephrotic proteinuria, microhematuria, and renal failure (42.5%) and close to 8% of pure nephrotic syndrome. The presence of renal failure regardless of other abnormalities in urinalysis showed a trend toward IgA nephropathy. Membranous nephropathy may have a more varied presentation than was originally thought and IgA nephropathy presenting as nephrotic syndrome with varying combinations of sediment may not be uncommon. The sediment-based breakdown of major glomerular diseases in our study is shown in Table 2.

The prevalence of native kidney disease varies according to the geographic area, socioeconomic condition, race, age, demography, and indication of renal biopsy. A comparison between our study and other Indian studies is shown in Table 3. However, we were unable to find corresponding studies classifying native kidney disease according to urine sediment and their histopathological correlation, and as to our knowledge, this is the first study to classify renal disease in this manner.

The profile of patients with diabetes with and without diabetic nephropathy is as follows: 89 patients with diabetes were biopsied, 15 (16.8%) had histopathological evidence of pure diabetic nephropathy, 45 (50.5%) had no diabetic nephropathy, and 29 (32.5%) had diabetic nephropathy along with a nondiabetic disease. Postinfectious glomerulonephritis was the major glomerular disease in the latter group [Figure 11]. IgA nephropathy (22.2%) and membranous nephropathy (15.5%) were the major diseases in patients with diabetes with no diabetic nephropathy [Figure 11]. Other diseases in biopsied patients with diabetes included MCD, pauci-immune glomerulonephritis, amyloidosis, FSGS, lupus nephritis, and acute interstitial nephritis [Figures 10 and 11]. Nondiabetic renal disease (NDRD) is seen as a cause of proteinuria and renal failure in type 2 diabetes mellitus. The clinical differences between NDRD and diabetic glomerulosclerosis are not clear. Other studies have shown MCD, vasculitis, or IgA nephropathy with 20%–25% of patients with diabetes have NDRD.[1819]
The pediatric population formed 15.4% of our sample size. They were also analyzed similarly. Major differences from the general population were the predominance of MCD in Groups I and II (MCD and membranous nephropathy in general population) and the predominance of lupus nephritis in Group V (IgA nephropathy in general population). Other pediatric studies have shown predominant FSGS, IgA nephropathy, MCD, lupus nephritis, and HSP nephritis as being major causes of pediatric renal disease.[2021]
Renal failure with proteinuria formed a small percentage of biopsied diseases [Figure 11]. In this group also, membranous nephropathy and MCD dominated the nephrotic syndrome group, thus establishing their presence throughout all combinations of nephrotic syndrome. IgA nephropathy, lupus nephritis, and acute interstitial nephritis comprised the other group with renal failure (subnephrotic proteinuria). We observed that regardless of presentation, IgA nephropathy was the predominant disease in the presence of renal failure (Groups III, V, and VII) as well as the predominant NDRD in patients with diabetes without biopsy-proven diabetic nephropathy. The incidence of acute kidney injury in IgA nephropathy is rare (<5%), but renal failure may be present in established IgA nephropathy. In this setting, the presence of renal failure irrespective of urinalysis finding may be a significant predictor for IgA nephropathy.[22]
Conclusions
The analysis of urinary sediment and renal failure is a useful tool in assessment of renal disease. In our study, we observed that the presence of renal failure regardless of other abnormalities in urinalysis showed a trend toward IgA nephropathy. Membranous nephropathy may have a more varied presentation, with microhematuria and renal failure, than was originally thought and IgA nephropathy presenting as nephrotic syndrome may not be uncommon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Characterization of kidney lesions in Indian adults: Towards a renal biopsy registry. J Nephrol. 2006;19:205-10.
- [Google Scholar]
- Spanish Registry of Glomerulonephritis. Clinicopathologic correlations of renal pathology in Spain. Kidney Int. 2004;66:898-904.
- [Google Scholar]
- Changing etiologies of unexplained adult nephrotic syndrome: A comparison of renal biopsy findings from 1976-1979 and 1995-1997. Am J Kidney Dis. 1997;30:621-31.
- [Google Scholar]
- Changing incidence of glomerular diseases in adults. Am J Kidney Dis. 2000;35:878-83.
- [Google Scholar]
- Epidemiologic data of primary glomerular diseases in Western France. Kidney Int. 2004;66:905-8.
- [Google Scholar]
- Paulista registry of glomerulonephritis: 5-year data report. Nephrol Dial Transplant. 2006;21:3098-105.
- [Google Scholar]
- Primary glomerular diseases in Brazil (1979-1999): Is the frequency of focal and segmental glomerulosclerosis increasing? Clin Nephrol. 2004;61:90-7.
- [Google Scholar]
- The Italian experience of the national registry of renal biopsies. Kidney Int. 2004;66:890-4.
- [Google Scholar]
- Adult minimal-change disease: Clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol. 2007;2:445-53.
- [Google Scholar]
- Histopathology of lupus nephritis: A single-center, cross-sectional study from Karnataka, India. IJRCI. 2014;2(S1):OA3.
- [Google Scholar]
- Clinical value of renal biopsy in patients with asymptomatic microscopic hematuria with and without low-grade proteinuria. Clin Nephrol. 2004;62:267-72.
- [Google Scholar]
- Glomerular disease as a cause of isolated microscopic haematuria. Q J Med. 1994;87:329-35.
- [Google Scholar]
- Nondiabetic kidney disease in type 2 diabetic patients: A single center experience. Indian J Nephrol. 2012;22:358-62.
- [Google Scholar]
- Non-diabetic renal disease (NDRD) in patients with type 2 diabetes mellitus (type 2 DM) J Assoc Physicians India. 2013;61:194-9.
- [Google Scholar]
- Should ultrasound guided percutaneous renal biopsy in children be done in a day care setting? Indian J Nephrol. 2010;20:21-4.
- [Google Scholar]
- Indications and results of renal biopsy in children: A 10-year review from a single center in Serbia. J Nephrol. 2012;25:1054-9.
- [Google Scholar]
- Pattern of biopsy-proven renal disease in a single center of South India: 19 years experience. Indian J Nephrol. 2011;21:250-7.
- [Google Scholar]
- Spectrum of biopsy proven renal disease and changing trends at a tropical tertiary carecentre1990-2001. Indian J Nephrol. 2003;13:29-35.
- [Google Scholar]







