Translate this page into:
Monoclonal Gammopathy of Renal Significance Presenting as Cryoglobulinemic Glomerulonephritis: A Case Report and Review of Literature
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Monoclonal gammopathy of renal significance (MGRS) can present with myriad of morphological features. We report a case of MGRS in a 46-year-old man who presented with nephrotic-range proteinuria and renal insufficiency. Renal biopsy showed amorphous eosinophilic periodic acid–Schiff positive deposits in capillary loops and lamda light chain positivity on immunofluorescence, suggestive of cyoglobulinemic glomerulonephritis. Serum cryoglobulins were positive. Serum immunoelectrophoresis and immunofixation showed a M band of 0.5 g/dl of IgG lambda type. Bone marrow showed 8% of plasma cells which confirmed the diagnosis of MGRS.
Keywords
Cryoglobulinemia
kidney biopsy
monoclonal gammopathy of renal significance
Introduction
Evidence of light chain cast nephropathy on renal biopsy is an absolute sign of multiple myeloma presenting with overt renal failure and necessitates chemotherapy.[1] However, monoclonal gammopathy of unknown significance (MGUS) or smoldering myeloma really was not treated with chemotherapy in view of the absence of end organ damage. MGUS, by definition, shows monoclonal protein of <3 g/dl and <10% plasma cells in bone marrow.[2] Recently, it has been shown that even these small amounts of paraprotein can result in renal failure and respond to chemotherapy and is called monoclonal gammopathy of renal significance (MGRS).[34] There are myriad of morphologic features of MGRS. We present one such case of MGRS in a 46-year-old male, who presented like cryoglobulinemic glomerulonephritis.
Case Report
A 46-year-old male with no prior history of renal complications came with complaints of pedal edema and facial puffiness. Routine blood and urine examination revealed the following results. Hemoglobin 10.5 gm/dl, total leukocyte count 5700 cells/mm3, platelets 2.5 lakh/mm3, serum creatinine 2.4 mg/dl, urea 40 mg/dl, sodium 138 mmol/L, potassium 4.4 mmol/L, chloride 100 mmol/L, calcium 8.5 mg/dl, uric acid 5.4 mg/dl, phosphorus 3.1 mg/dl, total proteins 5.3 g/dl, albulin 2.7 g/dl, serum glutamic oxaloacetic transaminase 21U/L, serum glutamic-pyruvic transaminase 24U/L, ALP 106U/L, LDH 240 IU/L, and 24 h urine protein 8 g/day with no hematuria. He was known hypertensive for the past 3 months using a single antihypertensive, amlodipine 10 mg daily with blood pressure maintaining at 130/80 mm/Hg. Serum rheumatoid factor (RA), antinuclear antibody, dsDNA, antineutrophil cytoplasmic antibody, and Coomb's test showed negative results. Serum C3 and C4 complement levels were normal. HIV, HAV, HBV, HCV, HEV, and tuberculosis infections were ruled out. In view of abnormal serum creatinine and nephrotic range proteinuria, he subsequently underwent renal biopsy.
Renal biopsy was adequate with 12 glomeruli. The glomeruli were enlarged and all the capillary loops were plugged with amorphous eosinophilic periodic acid–Schiff positive deposits Figure 1a and b]. The glomerular basement membrane showed reduplication [Figure 1c]. The tubulointerstitium was mostly unremarkable but for minimal lymphomononuclear infiltrate in interstititum. The vessels were normal. Immunofluorescence (IF) revealed only lambda light chain positivity in the glomerular deposits [Figure 1d]. The presence of these monoclonal deposits further warranted bone marrow examination. Bone marrow aspirate was particulate with normal cellularity, myeloid erythroid ratio of 3:1, and mild prominence of plasma cells accounting for 8% of nucleated cells. Trephine biopsy features were consistent with normal marrow. Serum cryoglobulins were positive. Serum protein electrophoresis has shown M-spike with M-protein of 0.5 g/dl in the gamma region. Serum Agar gel immunofixation electrophoresis had shown the presence of monoclonal immunoglobulin IgG class with lambda light chains. Urine immunofixation was also positive for paraprotein of IgG–lambda type. There was no evidence of lytic lesions on skeletal survey by X-ray. Quantitative tests for IgG, IgA, IgM, and IgE revealed hypogammaglobulinemia-IgG 665 mg/dl (800-1700), IgA 45 mg/dl (100–490), IgM 6 mg/dl (50–320), and IgE 151 IU/ml (158 in adults). The free light chain (FLC) ratio, however, was normal (1.17). Constellation of all these features and investigations were consistent with a diagnosis of MGRS.
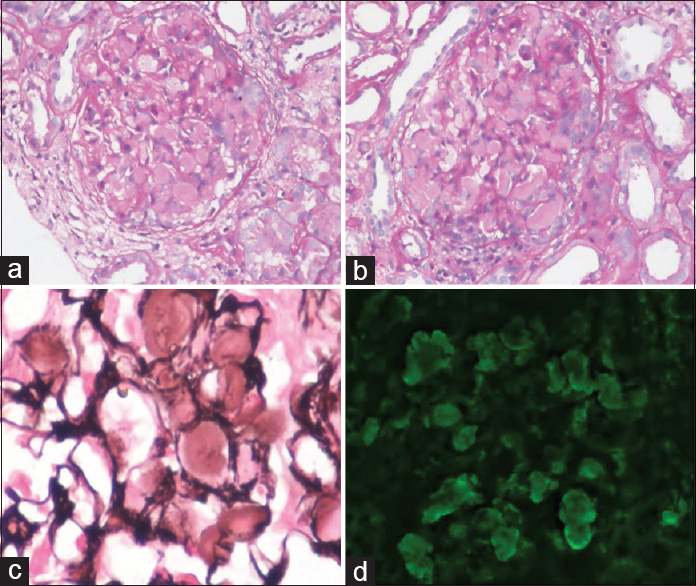
- (a and b) The enlarged glomeruli showing capillary loops plugged by periodic acid–Schiff positive deposits, PAS ×400. (c) Reduplication of glomerular basement membrane. SM-PASX400. (d) Lambda light chain positivity on immunofluorescence
Discussion
The genesis of this entity began with a publication by Sethi et al., wherein they described 28 hepatitis negative patients with monoclonal gammopathy and showing membranoproliferative pattern on renal biopsy.[5] MGUS was the most common association in these patients. Cryoglobulins were identified in 4 of their biopsies. However, light chain restriction was not seen in IF in any of them. This was followed by publication of more number of such cases and formation of well-defined entity called MGRS.[678] Bridoux et al. in their recent review have beautifully elaborated about the clinical, morphologic, and therapeutic nuances of this entity.[3] The clinical presentation of MGRS can vary from isolated proteinuria to end-stage renal disease. It is important to keep this diagnosis in mind, especially in elderly patients (>65 years) who present with proteinuria and unexplained renal failure. Renal biopsy forms an important startup point in the diagnosis of MGRS. The biopsy features of MGRS are classified according to the electron microscopic features as those showing organized versus nonorganized deposits. It can reflect on renal biopsy as amyloidosis, light chain deposit disease, fibrillary and immunotactoid glomerulonephritis, proximal light chain tubulopathy, or cryoglobulinemic glomerulonephritis. Uncommon features such as crystalloid glomerulopathy have also been reported.[6] However, cast nephropathy which is an overt manifestation of multiple myeloma is not included under MGRS.
Cryoglobulinemia is most commonly associated with hepatitis C virus infection. Mixed cryoglobulins (MCs) are proteins that reversibly precipitate at ≤37°C and consist of a mixture of monoclonal or polyclonal IgM that have antiglobulin (rheumatoid factor-RF) activity and bind to polyclonal IgG.[9] MCs are categorized as type II cryoblulinemia if the IgM RF is monoclonal, and as type III if IgM RF polyclonal. Renal involvement is reported in one-third of cryoglobulinemic patients and almost exclusively occurs in association with type II MC. Glomerular involvement occurs in 30% of patients with type I cryoglobulinemia.[10] Sethi et al. have reported cryoglobulinemia in hepatitis-positive as well as negative patients in their study.[5]
This should be remembered as an important morphologic pattern of MGRS to initiate the investigations for paraproteinemia, particularly in hepatitis-negative individuals. IF can be helpful in proving the monoclonality of these cryoglobulins similar to that seen in our patient. The laboratory workup for the diagnosis of monoclonal gammopathy is extensive and should include serum and urine immunofixation, bone marrow examination, and FLC assay. A combination of these tests is required instead of using a single measure like FLC since MGRS is associated with a small clone. The specificity of the tests varies according to the underlying morphology of MGRS. Nasr et al. has demonstrated all patients of MIDD had abnormal FLC whereas only 50% of patients with MPGN had abnormal FLC, but all showed abnormal results on immunofixation studies.[511] This can perhaps explain the normal FLC in our patient with M band on immunofixation. Much as the clinical and morphologic description, the therapeutic strategies of this entity are also well defined. Chemotherapy is mandatory in all patients and a combination of bortezomib and dexamethasone has shown promising results.[12] This patient was treated with three cycles of intravenous bortezomib and oral dexamethasone in standard dose recommendations. The patient is on irregular follow-up. Eight months after initiation of therapy, he was symptom-free. Serum creatinine and 24 h urine protein increased to 5.4 mg/dl and 9.1 g/day, respectively. Treatment in renal transplant also has been shown to be effective; however, with a risk of recurrence of the underlying B-cell clone if not effectively controlled. Biopsy proven posttransplant case has also been reported.[13]
Thus, we present a well worked up case of MGRS who presented with cryoglobulinemic glomerulonephritis. It is important to consider the diagnosis of MGRS in elderly patients presenting with proteinuria and unexplained renal failure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Renal disorders associated with monoclonal gammopathies: Diagnostic and therapeutic progress. Presse Med. 2012;41(3 Pt 1):276-89.
- [Google Scholar]
- Prevalence and risk of progression of light-chain monoclonal gammopathy of undetermined significance: A retrospective population-based cohort study. Lancet. 2010;375:1721-8.
- [Google Scholar]
- Diagnosis of monoclonal gammopathy of renal significance. Kidney Int. 2015;87:698-711.
- [Google Scholar]
- Monoclonal gammopathy of renal significance: When MGUS is no longer undetermined or insignificant. Blood. 2012;120:4292-5.
- [Google Scholar]
- Membranoproliferative glomerulonephritis secondary to monoclonal gammopathy. Clin J Am Soc Nephrol. 2010;5:770-82.
- [Google Scholar]
- Crystalloid glomerulopathy in monoclonal gammopathy of renal significance (MGRS) Clin Kidney J. 2014;7:296-8.
- [Google Scholar]
- Monoclonal gammopathy of renal significance: Why is it significant? J Blood Disord. 2014;1:2.
- [Google Scholar]
- Crystalglobulinemia syndrome due to monoclonal gammopathy of renal significance. QJM. 2015;108:417-8.
- [Google Scholar]
- Hepatitis C virus-related cryoglobulinemia and glomerulonephritis: Pathogenesis and therapeutic strategies. Ann Ital Med Int. 2005;20:71-80.
- [Google Scholar]
- Renal involvement in hepatitis C infection: Cryo-globulinemic glomerulonephritis induced by hepatitis C virus. Kidney Int. 1998;54:650-71.
- [Google Scholar]
- Renal monoclonal immunoglobulin deposition disease: A report of 64 patients from a single institution. Clin J Am Soc Nephrol. 2012;7:231-9.
- [Google Scholar]
- How I treat monoclonal gammopathy of renal significance (MGRS) Blood. 2013;122:3583-90.
- [Google Scholar]
- Monoclonal gammopathy of renal significance with light-chain deposition disease diagnosed postrenal transplant: A diagnostic and therapeutic challenge. Transpl Int. 2015;28:375-9.
- [Google Scholar]







