Translate this page into:
Acute Pyelonephritis: A Single-center Experience
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute pyelonephritis (APN), although a common clinical entity, still not much is known about the clinical profile in the Indian scenario. We prospectively collected clinical, biochemical, and radiological data of patients hospitalized with a diagnosis of APN from March 2014 to June 2016. A total of 296 cases were included in the study. Mean age was 53.85 ± 9.78 years. Male to females ratio was 1.93:1. Among the risk factors recognized for complicated pyelonephritis (PN), diabetes mellitus (DM) (54.4%) was the most common factor followed by renal calculi (14.4%), benign prostatic hyperplasia (6.7%), immunocompromised state (3.3%), stricture urethra and meatal stenosis (3.3%), and neurogenic bladder (2%). Urinary culture was negative in 153 (51.7%) and positive in 143 patient (48.3%). Most common organism isolated was Escherichia coli (29.7%), followed by Klebsiella pneumoniae (5.4%), pseudomonas (5.4%), Enterococcus (4.4%), and Proteus in 10 (3.4%). Serum creatinine of more than 1.5 mg/dl at admission was seen in 96.3% patients; 40% of them had underlying chronic kidney disease with DM being the most common. Multiorgan dysfunction either at admission or during the course in hospital stay was seen in 31.8% patients. Twelve (2%) had emphysematous PN. Six patients had Class II, 4 had Class III, 1 with Class I, and another with Class IV. A total of 18 deaths were noted (6.1%). Hemoglobin <10 g/dl, serum creatinine at admission >1.5 mg/dl, HbA1c% >10%, and immunosuppression had statistically significant association with the development of multiorgan dysfunction on univariate analysis, but on multivariate analysis, only hemoglobin, HbA1c%, and immunosuppression reached statistical significance. Even with attributable risk of mortality, only hemoglobin, HbA1c%, and immunosuppression reached statistical significance on multivariate analysis. HbA1c% adds to the predictive parameters to recognize at-risk patients to intensify the treatment and avoid complications.
Keywords
Computed tomography
diabetes mellitus
emphysematous pyelonephritis
HbA1c%
multiorgan dysfunction
pyelonephritis
Introduction
Acute pyelonephritis (APN) is a well-known disease, described extensively in literature. Earliest citing of the condition dates back to ancient Egypt, highlighting the destruction of the kidney parenchyma and its outcomes.[1] In spite of this long history, the nomenclature of APN is still controversial, and the semantic ambiguities can still cause confusion.
APN in the USA has an incidence as high as 250,000 cases per year and requires 100,000 hospitalizations every year.[2] In a recent large cohort in a community-based study, on average per year among 1000 patients, there were 152.7 lower respiratory tract infections (95% confidence interval [CI] 151.3–154.1) and 99.6 urinary tract infections (UTIs) (95% CI 98.4–100.8).[3] The absolute number of deaths in 28 days after the diagnosis of UTIs was still high compared with those after sepsis because of the higher incidence rate of UTIs. It was interesting that a high proportion of hospitalizations within 28 days were not on the day of diagnosis. This could reflect high underlying hospitalization rates in this cohort or could be attributable to exacerbation of underlying comorbidities by acute infections.[3] The considerable number of hospitalizations within 4 weeks of lower respiratory tract infections and UTIs with a cardiovascular cause of admission are particularly intriguing, as both infections have been found to exacerbate underlying cardiovascular comorbidity.[4] Hence, identification of the novel prognostic markers for this ancient disease is the need of hour to triage those with the risk of adverse outcomes.
It is essential to define the clinical, biochemical, and radiological profile of patients with APN to identify the early prognostic markers so as to prevent the morbidity and mortality. However, there are no Indian studies addressing these issues of incidence, prevalence, and risk factors. Our goal was to assess the relationship between the clinical laboratory data at presentation and adverse outcomes.
Materials and Methods
Study design, population, and settings
We prospectively collected all patients hospitalized at our tertiary care hospital from March 2014 to June 2016 with a diagnosis of pyelonephritis (PN) aged more than 14 years. The clinical features and laboratory data at the initial presentation, management, and outcomes were collected prospectively.
Definitions
-
APN was defined as the presence of two of the following: (a) axillary temperature ≥38.3°C or chills; (b) flank pain or costovertebral angle tenderness or pain on bimanual palpation of the kidney; and (c) mictional syndrome (including two or more of the following; dysuria, frequency, suprapubic pain, or urgency) together with the presence of pyuria (a positive leukocyte esterase dipstick test result, subsequently confirmed by urinalysis with more than ten leukocytes/mL in urine without centrifuging or more than five leukocytes per high-power field in centrifuged sediment) or a positive urine culture
-
Complicated PN was defined as PN occurring in any male patient, in patients with functional or anatomical abnormalities of the urinary tract, immunosuppressed persons, patients with a single kidney, permanent bladder catheter, nephrostomy, or double-J catheter, or those patients who had experienced urinary tract manipulation in the previous 2 weeks
-
The criteria for systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic shock were established according to the SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference.[5] SIRS was defined as the presence of two or more of the following conditions: fever (axillary temperature >38.3°C) or hypothermia (<36°C), tachypnea (>24 breaths/min), tachycardia (heart rate >90 beats/min), leukocytosis (>12,000 cells/mL), leukopenia (<4000 cells/mL), or >10% bands
-
Patients were considered to have sepsis if they had the criteria for SIRS and a clinical or microbiologically verified infection
-
Severe sepsis was defined as sepsis associated with hypoperfusion abnormalities such as prerenal azotemia, oliguria, altered mental status, acrocyanosis and/or coldness, or hypotension
-
Septic shock was defined as sepsis with a systolic blood pressure <90 mmHg or 40 mmHg less than the patient's baseline blood pressure for at least 1 h, despite adequate fluid resuscitation
-
Multiple organ dysfunction syndrome (MODS): dysfunction of more than one organ, requiring intervention to maintain homeostasis
-
Emphysematous pyelonephritis (EPN) was defined as based on the presence of gas in the renal parenchyma, collecting system, or perinephric tissue. On the basis of computed tomography (CT) scan, patients were classified into the following classes: (1) Class I: gas in the collecting system only, (2) Class II: gas in the renal parenchyma without extension to the extrarenal space, (3) Class IIIA: extension of gas or abscess to the perinephric space; Class IIIB: extension of gas or abscess to the pararenal space, and (4) Class IV: bilateral EPN or solitary kidney with EPN
-
Renal abscess: clinical manifestations of renal and perinephric abscess were similar to those of APN. Imaging studies were done to localize abscess
-
Renal dysfunction: presenting serum creatinine >1.5 mg/dl
-
Urine culture positive: >103 colony forming units/ml of bacteria were found
-
CT was diagnostic of PN if single or multiple hypodense areas were evidenced after contrast medium injection along with above mentioned clinical features
-
Glycemic control was defined as good if HbA1c <7%, moderate if HbA1c 7%–7.5%, and poor if HbA1c >7.5%
-
Defervescence was defined as the time needed for the axillary temperature to be <37°C in the presence of clinical improvement
-
Therapeutic failure was considered to be the persistence or worsening of the symptoms after 5 days of adequate treatment
-
Relapse was defined as the presence or the reappearance of symptoms or signs of the infection with the same microorganism within 4 weeks after discontinuation of the antibiotic treatment and reinfection as recurrence due to a different bacterial strain.
Exclusion criteria
Patients were excluded from the study if they were in the postoperative period after major urological surgery, had a kidney transplant, or were pregnant.
Management
Patients were treated with antibiotic as per culture sensitivity reports. Patients with non-EPN (NEPN) were treated with parenteral antibiotics for 1 week followed by oral antibiotics for 2 weeks and EPN patients received antibiotics for at least 3 weeks. Percutaneous drainage (PCD) with pigtail or percutaneous nephrostomy tube was inserted into pelvis or perirenal space to drain out fluid collection/gas in addition to antibiotics. Nephrectomy was carried out in patients refractory to antibiotics, PCD, and/or clinical deterioration. Outcomes were divided as those developing multiorgan dysfunction or death or discharge serum creatinine more than 1.5 mg/dl.
Statistical methods
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on mean ± standard deviation (minimum–maximum) and results on categorical measurements are presented in number (%). Significance is assessed at 5% level of significance. Student's t-test (two-tailed, independent) has been used to find the significance of study parameters on a continuous scale between two groups (intergroup analysis) on metric parameters. Chi-square/Fisher's exact test has been used to find the significance of study parameters on a categorical scale between two or more groups.
Significant figures
+Suggestive significance (p value: >0.05<0.10)
*Moderately significant (p value:0.01-0.05)
**Strongly significant (p value <0.01).
Statistical software
The statistical software, namely, SAS 9.2 (SAS Institute, Cary, NC) SPSS 15.0 (SPSS, Inc., Chicago, IL), Stata 10.1 (College Station, TX: SataCorp LP), MedCalc 9.0.1 (MedCalc Software, Ostend, Belgium) Systat 12.0 (Systat Software, San Jose, CA), and R environment version 2.11.1 (R Foundation for Statistical Computing in Vienna, Austria) were used for the analysis of the data, and Microsoft Word and Excel have been used to generate graphs and tables.
Results
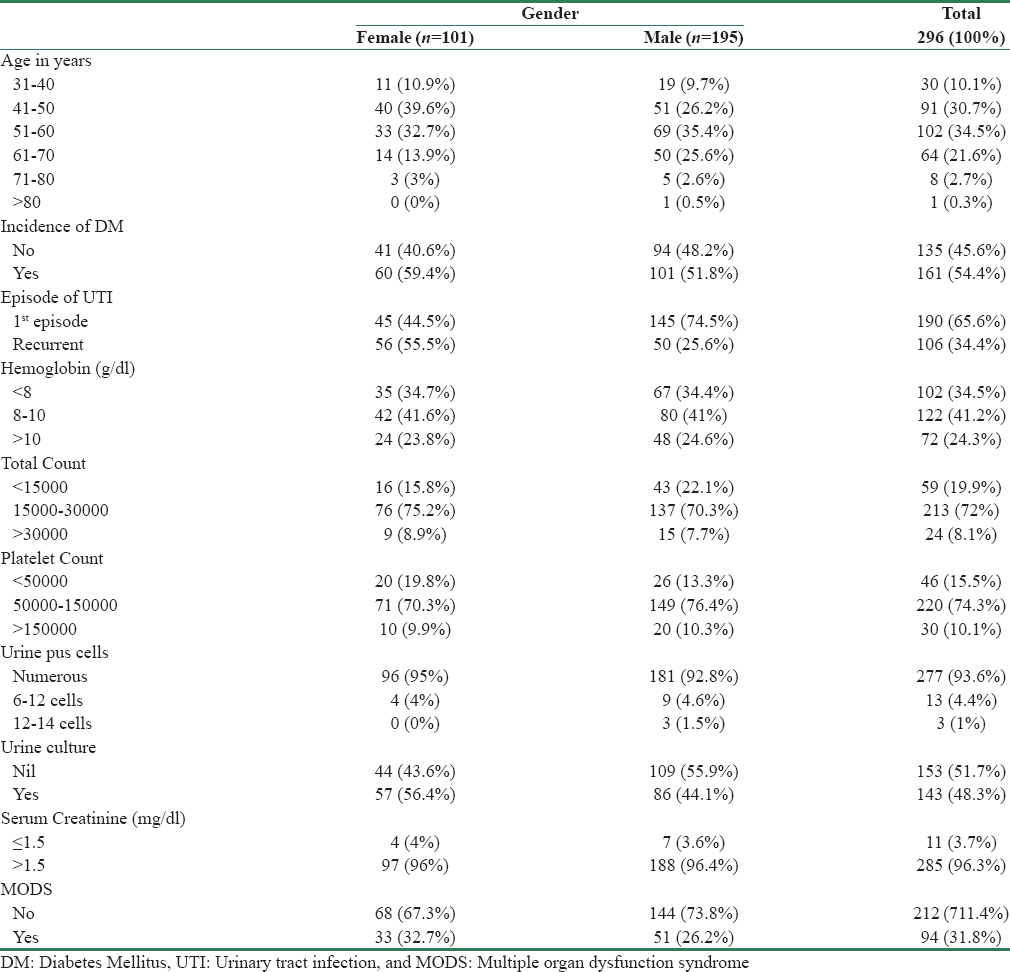
We collected a total of 296 cases over a period of 2 years. Mean age of the patients was 53.85 ± 9.78 years. One hundred patients (33%) were admitted in Intensive Care Unit (ICU). Males outnumbered females, 195/296 (65.9%) and 101/296 (34.1%), respectively. Baseline clinical, laboratory, and microbiological characteristics are shown in Table 1. One hundred and forty-five patients (54.4%) were known diabetic. It was the first episode of APN in 190 (65.6%) patients, the remaining 106 (35.4%) had experienced previous episodes; recurrent UTI patients had diabetes in 66 (62%) patients, and chronic kidney disease (CKD) in another 30 (28%) patients.
Hemoglobin of <10 g/dl was noted in 224 (75.7%) patients with 102 (34%) having <8 g/dl. Subgroup analysis showed about 67% of those with hemoglobin <10 g/dl had underlying CKD at presentation. Leukocytosis was evident in 237 patients (80%); mean leukocyte count was 21572.02 ± 8269.74. Leukocytes normalized in 5.6 ± 2.4 days.
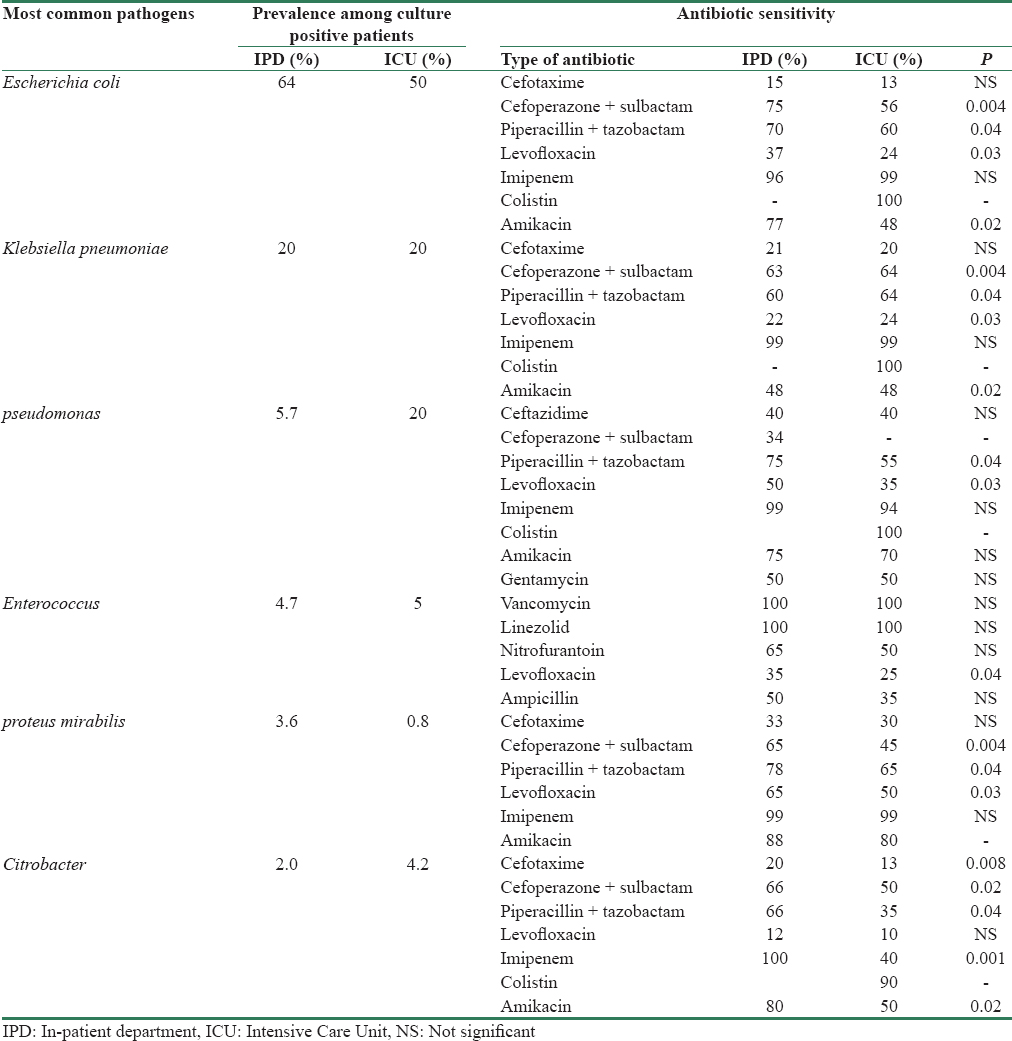
Pyuria was noted in 100% of cases. Urinary culture was negative in 153 (51.7%) and positive in 143 (48.3%) cases. Most common organism isolated was Escherichia coli in 88 (29.7%), followed by Klebsiella pneumoniae in 16 (5.4%), pseudomonas in 16 (5.4%), Enterococcus in 13 (4.4%), and Proteus in 10 (3.4%) [Figure 1]. Antibiogram of the most common organism is shown in Table 2. There was no difference in the prevalence of organisms in inpatient department (IPD) and ICU except for isolation of Citrobacter in ICU; there was an increasing trend in antibiotic resistance to common antibiotics used in ICU as against those in IPD patients. E. coli was sensitive to cefotaxime in only 15%, piperacillin-tazobactam in 75% in IPD patients as against 56% in ICU (p = 0.04), and levofloxacin sensitivity noted only 37% in IPD and 24% in ICU (p = 0.03). There has been a rise in the incidence of Citrobacter, with sensitivity to cefotaxime only 20%, 66% in IPD and 35% in ICU (p = 0.04), levofloxacin only 12% sensitive in IPD and 10% in ICU. However, there was an alarming increase in resistance to imipenem in ICU patients with only 40% sensitivity as against 100% in IPD (p = 0.001).

- Microorganisms grown in urine culture
Serum creatinine more than 1.5 mg/dl at admission was seen in 285 (96.3%) patients [Table 1]; 120 (40%) of them had underlying CKD with diabetes mellitus (DM) being the most common cause. Mean serum creatinine at admission was 4.95 ± 2.70 mg/dl. One hundred and two out of 285 (35.4%) patients required dialysis after admission; out of which, 78 of them were dialysis free at discharge. Distribution of HbA1c% in the different range is presented in Figure 2.

- HbA1c distribution of patients studied
Ninety cases (30%) were admitted in ICU. Multiple organ dysfunction syndrome (MODS) either at admission or during the course in hospital stay was seen in 94 (31.8%) patients. Eighty-seven (30%) patients with NEPN group and seven (60%) of EPN group had MODS at admission or during the course of hospital stay.
Risk factors categorizing the cases as complicated PN are presented in Table 3. Among the risk factors recognized for complicated PN, DM (54.4%) was the most common factor followed by renal calculi (14.4%), benign prostatic hyperplasia (6.7%), immunocompromised state (3.3%), stricture urethra and meatal stenosis (3.3%), and neurogenic bladder (2%) [Table 3]. In 153 patients with negative urine cultures, CT was positive for APN in 99.1%. Majority of these negative cases were attributed to the prior use of antibiotic therapy either at outside hospital or in-house use of antibiotic before sampling for cultures. Concordance between blood and urine cultures was only 20% in our study.

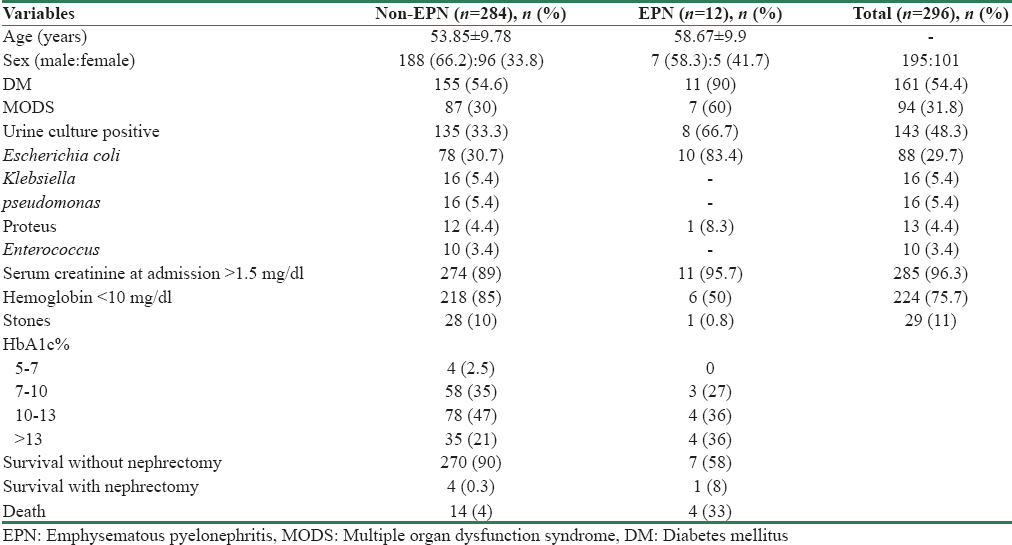
Ultrasonography showed abnormality in 67 (22.6%) patients; 12 of the 296 patients submitted to CT (2%) showed EPN. Six out of twelve patients had Class II, four had Class III, one with Class I, and another with Class IV. Prevalence of E. coli increased in EPN patients to 10/12 (83.4%). Compared to NEPN patients, EPN patients had a higher incidence of DM, 54% and 90% (p = 0.015), respectively; higher risk of developing MODS (p = 0.003). Four out of twelve (33%) EPN patients died and 1/12 (8%) underwent nephrectomy [Table 4].
Fifteen patients evaluated had a renal abscess on CT-kidney, ureter, and bladder. Subgroup analysis showed that there was no difference noted between patients with or without abscesses with regard to leukocytosis, duration of symptoms, urine cultures, and pyuria. Ultrasound examination showed abscess only in 2/15 cases. Patients with abscesses were more likely to be hospitalized for a longer time (20 ± 4.9 vs. 10 ± 3.3 days) and were more likely to be treated for a longer time. Two patients had renal vein thrombosis following APN on the same. Both of them had an extensive workup for prothrombotic state which was negative. Eventually, both had venous infarction of the affected kidneys with reduced renal function.
A total of 18 deaths were noted in 296 patients (6.1%). Hemoglobin <10 g/dl, serum creatinine at admission >1.5 mg/dl, HbA1c% >10%, and immunosuppression had statistically significant association with the development of MODS on univariate analysis, but on multivariate analysis, only hemoglobin, HbA1c%, and immunosuppression reached statistical significance. Even with attributable risk of mortality, only hemoglobin, HbA1c%, and immunosuppression reached statistical significance on multivariate analysis [Table 5].

Discussion
There has been a steady increase in the frequency of this disease in recent times, yet we do not have literature evidence regarding the risk factors, prognostic markers, and outcomes. Moreover, not all our patients had positive urine culture; and each episode of UTI adds to the renal damage and progression of CKD. It also precipitates or aggravates the underlying cardiovascular disease. Males outnumbered females in Indian studies in contrast to those Western studies [Table 6];[678] probably, reflecting the local gender differences in seeking hospital care. DM (54.4%) formed a single most important risk factor for categorizing as complicated PN. This emphasizes the fact that India being the capital of DM would likely to contribute more burden of PN in the future to the health-care system.

Urine culture was positive in only 48% of cases in our study [Table 1], but large variation has been noted in different study groups depending on the local practices. In our study, a large number of culture negativity was attributed to prior antibiotic usage either at outside hospitals before referral or to the late collection of samples. Subgroup analysis of these culture negative groups revealed that they are at lower risk of developing complications such as MODS, renal abscess, progression of renal failure, and death. Prevalence of organisms isolated was almost similar to those reported in other studies with E. coli being the most common organism in both EPN and NEPN groups, followed by K. pneumoniae. The most important intriguing finding in our study was differences in sensitivity pattern between inpatient in wards and intensive care patients although prevalence of organisms was same, there was more trend toward resistance to commonly used antibiotics (piperacillin-tazobactam, cefoperazone-sulbactam, and levofloxacin) in intensive care group [Table 2]. This emphasizes us to draw stringent antibiotic policies in hospitals to prevent further development of resistance to the latest antibiotic armamentarium and also to establish local antibiotic sensitivity patterns periodically and change in the usage of antibiotics accordingly.
Although ultrasonography is the most commonly used noninvasive radiological modality in the management of patients with APN, decision-taking process in APN is limited, which explains why many authors consider it unnecessary in this clinical setting when the patient progresses satisfactorily with adequate treatment, as is usually the case.[910] Notwithstanding this, the role of ultrasonography in the initial management of complicated PN has been poorly studied, which explains the lack of a wide consensus on this aspect. A previous prospective study involving 245 patients with febrile UTI found that ultrasonography detected 19.2% of clinically relevant urological disorders.[9] This figure is very different to that seen in our study bearing in mind that 66% of patients were diagnosed with APN. Although these authors propose a prediction rule to select the patients with PN who could benefit from an ultrasound study, we believe that given the high morbidity and high prevalence of alterations requiring urgent instrumentation, an ultrasonographic study should be performed in all APN patients. Furthermore, ultrasound was poor in detecting complications such as abscess, in which case CT was considered superior by a large number of studies. Thus, CT scan forms an important tool in the management of PN patients, particularly when expected clinical response is not seen.
The information available to date about the prognosis for acute and complicated PN and its influencing factors is scarce and limited to a very few particular settings.[67811] In our study, 31.8% of the patients developed MODS. Among the risk factors to predict MODS, univariate analysis showed statistical significance for hemoglobin <10 g/dl, serum creatinine more than 1.5 mg/dl at admission, HbA1c% more than 10%, and immunosuppression; but on multivariate analysis, statistical significance reached only with hemoglobin, HbA1c and immunosuppression [Table 4]. This analysis of HbA1c% is peculiar to our study and has not been reported in any of the previous studies.
Mortality associated with complicated PN ranges between 3.2% and 9.8%.[67811] Hemoglobin <10 g/dl, HbA1c% more than 10%, and immunosuppression were the factors that reached statistical significance in both univariate and multivariate analysis in predicting the mortality. Most of these factors have been previously identified in various studies as factors of poor prognosis.[79101112] Our study is unique in estimating the prognostic significance of HbA1c% in predicting the mortality.
Thus, in addition to the traditional markers of adverse outcomes, HbA1c% adds to our armamentarium in recognizing those at-risk patients. It also emphasizes us to stick to the basic tenet of better blood sugar control to reduce the incidence of these avoidable complications.
Our study has several limitations such as it did not include those with postoperative and posttransplant patients. This was done to represent those community-acquired PN cases. We also did not report the follow-up of these cases which require further studies in larger settings.
Conclusion
The absence of infected urine does not rule out the diagnosis of APN in common clinical practice. Local antibiogram pattern is essential to prevent further resistances in organisms. HbA1c% adds to the predictive parameters to recognize at-risk patients to intensify the treatment and avoid complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Dr.K.P. Suresh, Scientist (Biostatistics), National Institute of Veterinary Epidemiology and Disease Informatics (NIVEDI), Bangalore - 560 024.
References
- The clinical and imaging presentation of acute “noncomplicated” pyelonephritis: A new profile for an ancient disease. BMC NePhrol. 2011;12:68.
- [Google Scholar]
- Acute pyelonephritis in US hospitals in 1-997: hospitalization and in- hospital mortality. Ann Epidemiol. 2003;13:144-150.
- [Google Scholar]
- New estimates of the burden of acute community-acquired infections among older people with diabetes mellitus: A retrospective cohort study using linked electronic health records. Diabet Med. 2014;31:606-14.
- [Google Scholar]
- Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611-8.
- [Google Scholar]
- 2001 SCCM/ESICM /ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250-56.
- [Google Scholar]
- Acute pyelonephritis in diabetes mellitus: Single center experience. lndian J Nephrol. 2014;24:367-371.
- [Google Scholar]
- Acute pyelonephritis in adults: A case series of 223 patients. Nephrol Dial Transplant. 2012;27:3488-93.
- [Google Scholar]
- Clinical and epidemiologlcal features and prognosis of complicated pyelonephritis: A prospective observationalsingle hospital-based study. BMC Infectious. 2014;14:639.
- [Google Scholar]
- Managing uncomplicated urinary tract infection-making sense out of resistance data. Clin Infect Dis. 2011;53:1041.
- [Google Scholar]
- ECO.SENS. An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections:‘the ECO. SENS Project. J Antimicrob Chemother. 2003;51:69.
- [Google Scholar]
- The current management strategies for community-acquired urinary tract infectibn. lnfect Dis Clin North A. 2003;17:303-32.
- [Google Scholar]







