Translate this page into:
Crescentic Glomerulonephritis and Membranous Nephropathy: An Unusual Association
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 64-year-old female presented with the bilateral swelling of the legs. She had a history of high blood pressure seven months ago. At the time of the hypertension diagnosis serum creatinine was 1.1 mg/dl. The physical examination was unremarkable. Urinalysis showed 3+ red blood cells and 3+ protein. The amount of proteinuria was 7 g/day, serum creatinine at the time of admission was 2.7 mg/dl showing a progressive increase to 5.4 mg/dl over the next 1 week, serum albumin level was 2.1 g/dl, serum C3 was 0.9 g/L, and C4 was 0.3 g/L. Renal biopsy performed yielded cortex containing 10 glomeruli for light microscopy, of which 3 were globally sclerotic and the remaining 7 glomeruli had fibrous to fibrocellular crescents in all. No necrotic lesion was found. Capillary membranes were thickened with subepithelial spikes [Figure 1]. Direct immunofluorescence tests showed IgG, C3, and both kappa and lambda light chains granular deposits along the capillary walls. Immunostaining for anti-phospholipase A2 receptor (PLA2R) antibody was not performed. The histological diagnosis was crescentic glomerulonephritis (CGN) in association with membranous nephropathy (MN) stage II.
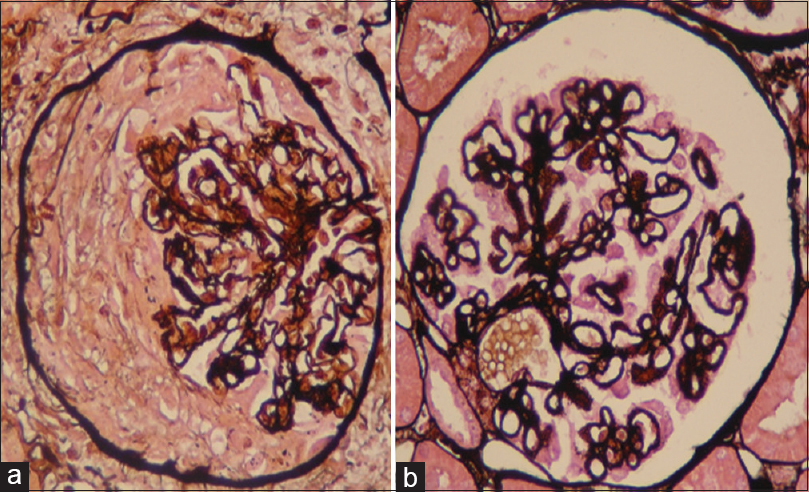
- (a) The glomeruli were involved by a fibrocellular crescent (H and E, ×400). (b) Silver stain shows basement membrane spikes (silver, ×400)
Antibody profile was negative for anti-double-stranded DNA, anti-neutrophil cytoplasmic antibody (ANCA), anti-glomerular basement membrane antibodies (anti-GBM), and PLA2R. Serology for hepatitis B and anti-hepatitis C virus antibody was negative. After evaluation for a secondary MN by chest abdominal computed tomography, colonoscopy, and duodenoscopy we found no evidence of cancer.
Treatment was initiated with 1 g of methylprednisolone intravenously daily for 3 days followed by prednisone per os daily 1 mg/kg/day for 1 month which was tapered down till discontinuation after 3 months. We also prescribed 1 g of intravenous cyclophosphamide (IVC). The patient was discharged 22 days after her admission, with creatinine level of 2.8 mg/dl. Five more monthly IVC doses were programmed. After 1 year follow-up, the patient referred no symptoms, her serum creatinine was 1.7 mg/dl, the 24 h urine protein was 1.5 g, urine sediment had no erythrocytes or casts, and ANCA was negative.
In the absence of lupus nephritis, anti-GBM nephritis or ANCA positive vasculitis, MN, and CGN is an unusual association.[1] In the best of our knowledge, there are 30 cases reported in the literature of concurrent MN, CGN, and negative ANCA serology [Table 1].[2] The largest series was reported by Rodriguez et al., in this none of the patients had extrarenal manifestation of vasculitis.[3]
| Author (year of publication) | Number of patients | Age (years) | Proteinuria (g/day) | Creatinine (mg/dl) | Treatment | ESRD |
|---|---|---|---|---|---|---|
| Kwan (1991) | 1 | 31 | 17 | 2.0 | Corticoide + cyclophosaphamide | Yes |
| James (1995) | 1 | 67 | 14.8 | 3.2 | Yes | |
| Tse (1997) | 6 | 55.6 (39-68) | 11.6 (0.4-22) | 5.85 (0.73-19.8) | Corticoide + cyclophosaphamide (5) Corticoide (1) |
No |
| Hall (2006) | 1 | 59 | - | 4.64 | Corticoide + cyclophosaphamide | No |
| Gadonski (2010) | 1 | 18 | 6.4 | 6.6 | Corticoide | No |
| Unver (2008) | 1 | 65 | - | 6.3 | Corticoide + cyclophosaphamide | No |
| Rodriguez (2014) | 19 | 55 (5-86) | 11.5 (3.3-29) | 2.9 (0.4-10) | Corticoide + cyclophosaphamide (8) Corticoide + mycophenolate mofetil (2) Cortcoide (1) None (3) |
4 |
ESRD: End-stage renal disease
This case may represent either an entity of MN with crescents or an MN with superimposed secondary ANCA-negative CGN.
ANCA-negative CGN tends to show necrotizing lesions in a context of systemic disease. In our case, the absence of necrotizing lesions in biopsy specimens and lack of extrarenal symptoms argue suggest that it could be a single distinct entity MN.
Moreover, it is not confirmed that our case is a primary MN, despite the negative screening for a secondary MN, in this context PLA2R immunostaining could be helpful. In all cases, the clinical course of this patient is serious and an immunosuppression is essential in order to avoid end-stage renal disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Membranous glomerulonephritis with ANCA-associated necrotizing and crescentic glomerulonephritis. Clin J Am Soc Nephrol. 2009;4:299-308.
- [Google Scholar]
- Crescentic glomerulonephritis and membranous nephropathy: A rare coexistence. Int Urol Nephrol. 2015;47:1373-7.
- [Google Scholar]
- Membranous nephropathy with crescents: A series of 19 cases. Am J Kidney Dis. 2014;64:66-73.
- [Google Scholar]






