Translate this page into:
The LE Cell—A Forgotten Entity
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 32 years old lady presented with progressive dyspnoea of 1 month that was associated with ankle edema, intermittent fever, polyarthralgia, and anorexia. Investigation revealed normocytic anemia, elevated erythrocyte sedimentation rate (ESR), nephrotic range proteinuria (spot urine protein creatinine ratio 5.6), normal renal function (serum creatinine 0.8 mg/dl), pericardial effusion with cardiac tamponade. Emergent pericardiocentesis was done. Pericardial fluid cytology is shown in Figure 1. Figure 2 represents buffy coat smear.
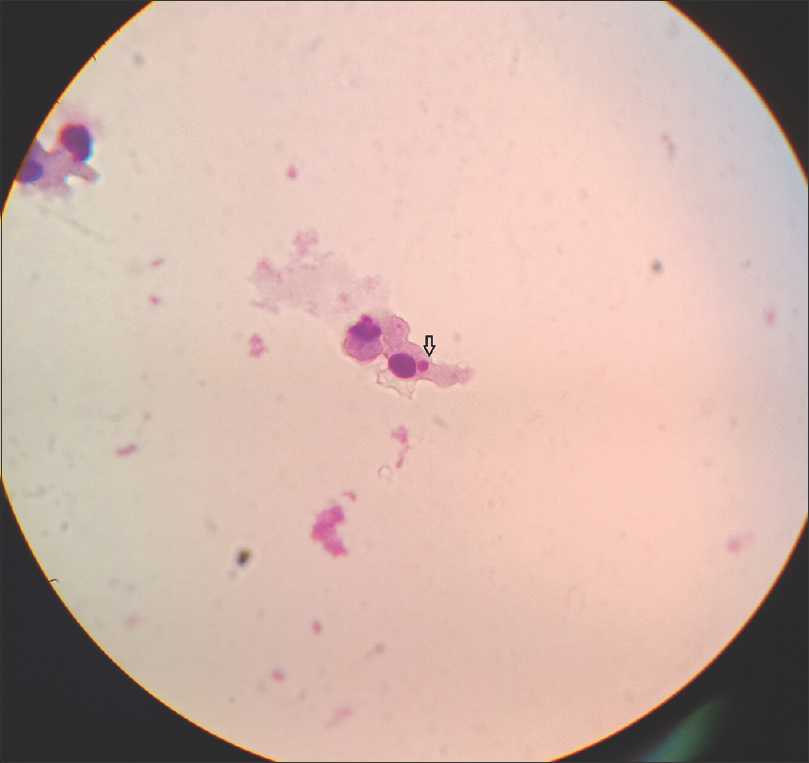
- Pericardial fluid cytology with Giemsa stain reveals the LE cell showing the characteristic Haematoxylin body (arrow)

- Buffy coat smear with Leishmann stain reveals the LE cell with characteristic LE body (arrow). Note that the native nucleus appears like a crescent and is eccentrically displaced
The Figures 1 and 2 demonstrate the presence of lupus erythematosus (LE) cell which is a neutrophil or monocyte having a single red-purplish amorphous inclusion known as haematoxylin or LE body (arrow) in the cytoplasm. LE body represents the degraded nuclear material of an injured cell which has been phagocytized by intact phagocyte. [1] LE cell is a telltale sign of autoimmune process. It results from phagocytosis of apoptotic bodies induced by autoantibodies and it is a hallmark of systemic lupus erythematosus (SLE). [2] LE cell can be identified in cytology (pleural/pericardial fluids), buffy coat or in histopathology specimen. LE cell is not normally seen in peripheral blood and, hence, defibrinated blood is chosen for promoting LE cell formation. This is done by shaking venous blood vigorously with glass beads or forcing clotted blood through a sieve. This ruptures the leukocyte and exposes the nuclear material. The sample is incubated at 37°C for the formation of LE cell and then centrifuged. Buffy coat is taken, smeared, stained, and examined. During incubation, the antinuclear antibodies in the serum bind to the exposed nuclear material and the whole complex is opsonized by the phagocytes resulting in the formation of LE cell. The process is referred to as LE cell phenomenon. Serum containing antinuclear antibody from patients with SLE can induce LE cell formation with donor blood sample. LE cells show crescentic band - like eccentrically placed nucleus. LE cell is not specific for SLE and it can be seen in autoimmune disorders such as rheumatoid arthritis, [3] drug-induced lupus etc., A cell that is morphologically similar to LE cell which could be encountered while examining bone marrow aspirates is “Tart Cell.” The tart cell is another phenotype of nucleophagocytosis and was first described by Hargraves et al. [1] The Tart cell can be seen as a normal finding in bone marrow smear; however, their numbers tend to be increased in SLE. Like the LE cell, the tart cell also has a phagocytosed nuclear material inside its cytoplasm, but the nuclear material retains its chromatin structure in Tart cell whereas the nuclear material in the LE cell has a homogeneous appearance. [1].
LE cell testing in buffy coat was previously used to diagnose SLE [4] but now it has been replaced by antinuclear antibody (ANA) testing. Compared to ANA testing LE cell testing is less sensitive for diagnosing SLE and it is labor intensive. However, it is relevant to be aware of this entity while interpreting cytology specimens. LE cell testing in buffy coat facilitates rapid diagnosis of SLE.
This patient had hypocomplementemia (low C3 and low C4) and ANA was positive with end point titer of 1:1280. Renal biopsy revealed class IV lupus nephritis. She was treated with intravenous pulse steroid therapy, intravenous cyclophosphamide followed by oral steroid therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Discovery of the LE cell and its morphology. Proc Staff Meet Mayo Clin. 1969;44:579-9.
- [Google Scholar]
- LE cells in the blood in acute disseminated lupus erythematosus. J Invest Dermatol. 1949;12:83-4.
- [Google Scholar]
- Rheumatoid arthritis and the positive L.E-cell phenomenon. Ann Rheum Dis. 1956;15:211-6.
- [Google Scholar]
- The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271-7.
- [Google Scholar]






