Translate this page into:
Clinical Utility of 24-h Ambulatory Blood Pressure Monitoring in Hospitalized Patients with Chronic Kidney Disease
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Hypertension leads to rapid progression of kidney disease. Hypertension (HTN) is the second most common cause for CKD after diabetes. Ambulatory blood pressure monitoring (ABPM) helps in accurate and early diagnosis of HTN along with measurements of other variables, namely nondippers, reverse dippers, hyperbaric index (HBI), percentage time elevation (PTE), and early morning surge.
Methodology:
After obtaining the institution ethics committee approval total 192 cases, of 12–80 years age group, who were diagnosed with CKD were included in the study. ABPM was done for patients using Meditech ABPM-05 machine.
Results:
Study showed male predominance. Maximum patients were in the age group of 41–60 years. Prevalence of Hypertension in patients with CKD was 88.02%. The systolic BP, diastolic BP, and mean arterial pressure (MAP) were significantly higher by clinic BP measurement than ABPM in all stages of patients with CKD especially in stage IV than stage V CKD. Systolic, diastolic, MAP, HBI and PTE at nighttime were significantly higher than daytime in all patients with CKD, especially in patients with resistant hypertension. Prevalence of whitecoat HTN (4.1%), whitecoat effect (16.1%), resistant hypertension (39.6%), masked HTN (1%), and masked uncontrolled HTN (10.4%) was noted. Systolic and diastolic HBI was lower in patients on hemodialysis as compared to those not on hemodialysis. Non-dippers were more than dippers.
Conclusion:
Apart from mean systolic and diastolic BP, ABPM gives the extent of end-organ damage and insights into the need for control of 24 h BP in patients of CKD.
Keywords
Ambulatory blood pressure monitoring
chronic kidney disease
clinical utility
Introduction
Chronic kidney disease (CKD) is an abnormality of kidney structure or function, present for >3 months. A study conducted by Rajapurkar et al. suggest that, in India, diabetes and hypertension accounts for 40%–60% cases of CKD.[1] In recent study, it has been found that hypertension is the second most common cause for CKD after diabetes only.[2] In current situation approximately 1 billion people worldwide have higher BP, which translates to about 1 of 4 adults being afflicted with hypertension.[3] Hypertension leads to rapid progression of kidney disease along with other complications, namely cardiovascular complication and cerebrovascular accidents, and hence, optimal control of BP will lead to a decrease in these complications.
Ambulatory BP Monitoring (ABPM) is a newer tool, which helps in accurate and early diagnosis of HTN along with measurements of other variables, namely non-dippers, reverse dippers, hyperbaric index (HI), Percentage Time Elevation (PTE) and Early Morning Surge (EMS), which can predict end-organ damage in hypertensive patients. Hence, we planned a study in patients with CKD to observe the prevalence and control of hypertension, and to study various blood pressure parameters. It has been observed that in India, ABPM study in CKD was published only in children and various single ABPM parameters are studied in adults. Also, in international literature, various components of ABPM have been studied individually; however, in our study we have compared various parameters of ABPM. Additionally, we have studied parameters of ABPM in patients with CKD with resistant hypertension separately.
Methodology
It was an observational prospective study conducted in tertiary care hospital after obtaining institutional ethics committee approval for a period of 18 months, from May 2017 to November 2018. Patients included in the study were diagnosed cases of CKD as per definition of KDIGO 2012 guidelines, who were admitted in general wards of tertiary care hospital. BP was measured by clinic method by mercury Sphygmomanometer. Two readings were measured at the interval of 5 minutes in both the upper limb and the average was taken as clinic BP. The ABPM cuff was applied on the arm (other than fistula hand) and the ABPM machine was tied at the level of waist with the help of belts. Two to three manual pilot readings were taken through ABPM machine. ABPM recordings of these patients were downloaded on a computer with EasyABPM software. ABPM was performed free of charge in the patients. ABPM readings were considered satisfactory if (1) >14 daytime readings and >7 nighttime readings. (2) >70% to 85% valid readings.
Whitecoat hypertension was defined as an office pressure of greater than 130/80 mmHg with a daytime home or ambulatory measurement of less than 130/80 mm of Hg.[4] The whitecoat effect was defined as the rise in BP that occurs in the medical environment regardless of the daytime ABPM level or the use of antihypertensive drugs.[4] Masked hypertension was defined as a normal blood pressure (BP) in the clinic or office (<130/80 mm Hg) but an elevated BP out of the clinic (ambulatory daytime BP or home BP >130/80 mmHg).[4] Masked uncontrolled hypertension (MUCH) was diagnosed in patients treated for hypertension who are normotensive in the clinic but hypertensive outside.[5] Dipper: dippers, the sleep-time BP mean is lower by 10% to 20% compared to the daytime mean.[6] Non-dippers: Absence of fall in BP <10% during sleep as compared to that of daytime values is defined as non-dipper.[6]
Hyperbaric impact was hypertension load calculated by ABPM machine, which provides information on how much time BP was higher than normal and how much it is higher than upper limit of normal ambulatory blood pressure during ABPM.[78] Percentage Time Elevation (PTE) was the proportion of time during which blood pressure values are higher than what is considered to be normal.[9]
Results and Summary
One hundred and ninety-two patients with age 12–80 years and satisfying inclusion criteria as per KDIGO 2012 were included. Pregnant females and patients with other secondary causes of hypertension were excluded. Sample size was calculated from the prevalence of hypertension in CKD, which was 43%. The study population was having 110 males (57.3%) and 82 (42.7%) females. Maximum number of cases, that is, 45.3% belongs to age group 41–60 years. In patients with CKD, 169 (88.02%) patients were found to have hypertension. The prevalence of controlled and uncontrolled blood pressure, whitecoat HTN, whitecoat effect, masked HTN, and masked uncontrolled HTN is depicted in Figure 1.
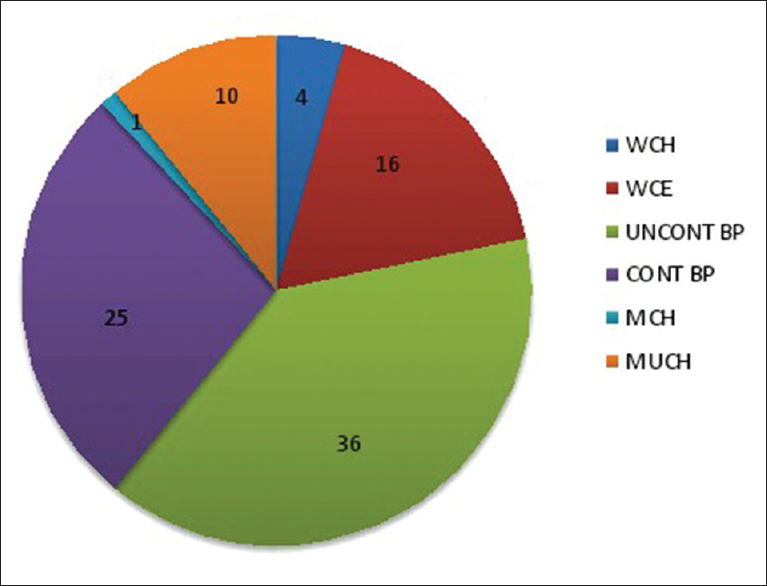
- Prevalence of controlled and uncontrolled BP, whitecoat HTN (WCH), whitecoat effect (WCE), masked HTN (MCH), and masked uncontrolled HTN (MUCH)
In all stages of patients with CKD, the mean clinic blood pressure measurements were significantly higher than mean ABPM measurements [Table 1]. In our study, it was observed that the nighttime systolic, diastolic, and MAP hyperbaric Index (HBI) (450.40 ± 34.28), (148.71 ± 16.83), and (222.02 ± 21.01), respectively, were significantly higher than daytime systolic, diastolic and MAP HBI (195.82 ± 19.95), (98.26 ± 13.16), and (115.76 ± 13.78), respectively, with P < 0.001.
| Parameters | Stage III (n=1) | Stage IV (n=18) | Stage V (n=173) | |||||
|---|---|---|---|---|---|---|---|---|
| ABPM | CBPM | ABPM | CBPM | P | ABPM | CBPM | P | |
| SBP | 115 | 150 | 136.11±23.57 | 147.22±28.52 | 0.001 | 129.52±21.13 | 136.53±25.90 | <0.001 |
| DBP | 69 | 90 | 78.28±17.80 | 88.00±18.47 | 0.006 | 75.79±14.18 | 81.87±15.16 | <0.001 |
| MAP | 84 | 110 | 97.56±19.52 | 107.74±21.08 | 0.003 | 93.60±15.60 | 100.09±17.72 | <0.001 |
| Pulse | 73 | 76 | 88.06±17.21 | 90.67±16.75 | 0.061 | 89.33±14.01 | 92.11±16.08 | <0.001 |
The mean nighttime hyperbaric index was significantly higher than daytime hyperbaric index in various stages of CKD especially stage IV CKD [Table 2]. In our study, we observed that patients on hemodialysis were having lower HBI than patients not on hemodialysis [Figure 2]. In patients with CKD, the nighttime systolic, diastolic, and MAP PTE were significantly higher than Daytime PTE, with P < 0.001 [Figure 3].
| HBI | Stage III (n=1) | Stage IV (n=18) | Stage V (n=173) | |||||
|---|---|---|---|---|---|---|---|---|
| Daytime | Nighttime | Daytime | Nighttime | P | Daytime | Nighttime | P | |
| Systolic HBI | 4 | 159 | 240.5±78.74 | 536.56±136.21 | <0.001 | 192.28±25.95 | 443.13±35.36 | <0.001 |
| Diastolic HBI | 9 | 75 | 134.67±61.79 | 184.56±73.91 | 0.029 | 94.98±13.15 | 145.41±17.09 | <0.001 |
| MAP HBI | 7 | 70 | 155.94±61.81 | 288.0±88.11 | 0.004 | 112.20±13.90 | 216.04±21.46 | <0.001 |

- Impact of hemodialysis on systolic HBI and diastolic HBI in patients with CKD (n = 192)
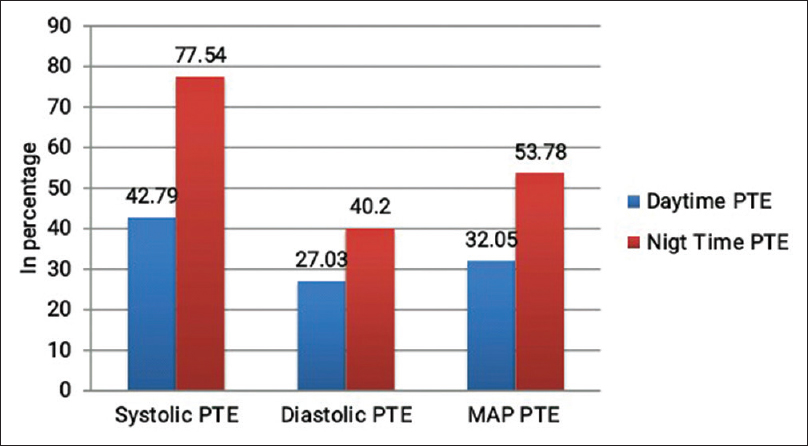
- Daytime and nighttime PTE in patients with CKD (n = 192)
In our study, we further classified patients with CKD into non-dippers and dippers as per nocturnal blood pressure. We found that, of total 192 patients, 162 (84.3%) patients were systolic non-dippers, while 148 (77.08%) were diastolic non-dippers and 160 (83.77%) patients were MAP non-dippers (P < 0.001).
The comparison of average daytime and nighttime SBP and DBP is given in Table 3. In 74 patients who were not on hemodialysis, 89.18% were systolic non-dippers and 81% were diastolic non-dippers as compared to 80.5% and 74.5% in patients on hemodialysis respectively. Prevalence of resistant hypertension in hypertensive patients with CKD was 39.6% (67 patients out of 169 hypertensive patients). Hyperbaric index and percentage time elevation in resistant hypertensive patients with CKD were significantly higher at nighttime than daytime [Table 4]. In our study, we found that hypertensive left ventricular hypertrophy 115 (59.8%) was the most common end-organ damage present in patients with CKD [Figure 4].
| Parameters | Nondippers (n=162) | Dippers (n=30) | P |
|---|---|---|---|
| Average Daytime SBP | 130.21±21.59 | 134.73±23.63 | 0.300 |
| Average Daytime DBP | 76.49±14.61 | 80.63±17.04 | 0.167 |
| Average Nighttime SBP | 130.04±23.94 | 117.9±22.84 | 0.011 |
| Average Nighttime DBP | 75.35±15.4 | 68.57±14.48 | 0.026 |
| Parameters | Nondippers (n=148) | Dippers (n=44) | P |
| Average Daytime SBP | 130.96±22.2 | 130.77±21.19 | 0.961 |
| Average Daytime DBP | 76.41±14.78 | 79.59±15.82 | 0.219 |
| Average Nighttime SBP | 131.25±24.46 | 117.7±19.88 | 0.001 |
| Average Nighttime DBP | 76.2±15.42 | 67.86±13.73 | 0.002 |
| Type | Daytime | Nighttime | P |
|---|---|---|---|
| Systolic HBI | 237.0±55.8 | 503.09±102.5 | <0.001 |
| Diastolic HBI | 89.02±22.3 | 136.4±40.2 | <0.001 |
| MAP HBI | 123.49±36.2 | 227.6±45.5 | <0.001 |
| Systolic PTE | 42.80±54.79 | 77.55±84.52 | <0.001 |
| Diastolic PTE | 27.04±32.10 | 40.20±38.55 | <0.001 |
| MAP PTE | 32.05±33.37 | 53.79±39.59 | <0.001 |

- Prevalence of other end-organ damage in patients with CKD (n = 192)
Discussion
This study was conducted in patients admitted in general medicine ward of a tertiary care hospital. The patients were predominantly having stage IV and stage V CKD. In our study, we observed the pattern of control of BP in patients with CKD over 24 hours, which helps us in diagnosing non-dippers, masked hypertension, resistant hypertension, and early morning surge in patients with CKD.
Age-wise distribution in total 192 patients showed maximum patients in the age group of 41- 60 years (i.e., 87 patients, 45.3%). It has been observed in the study by Iseki K et al. in 2005[10] also, that increasing age is a risk factor for progression of kidney disease. In patients with CKD, 169 (88.02%) patients were found to have hypertension. This finding is similar to CRIC study, where the prevalence of HTN in CKD was 86%, while that in general population it was 29%.[11] Study by Anchala R et al. showed that the prevalence of HTN in Indian population is 29.8%.[12] So, from the above results, it is clear that, patients with CKD have 3 time high burden of HTN as compared to the general population. Eighty patients were found to be diabetic; 39 females (47.5%) and 41 males (37.2%). TRIAD study found that diabetic females have higher prevalence of chronic kidney disease.[13]
Systolic, Diastolic BP and MAP measured by CBP were significantly higher than ABPM (<0.001). These results suggest that ABPM measures various parameters of BP more accurately than traditional CBP. In our study, it was observed that females had high SBP and DBP than male patients. Study by Tozawa M et al. showed that uncontrolled HTN was an independent risk factor for progression of renal disease.[14]
Total 91 patients were having BP above the target goals (which include uncontrolled HTN, MCH, MUCH), that is, the prevalence of uncontrolled HTN in CKD was 47.5%. It is important to note that out of these 91 patients, 22 patients were having normal Clinic BP, hence ABPM helps in the diagnosis of these patients with masked HTN, which can help treating physicians for optimizing the antihypertensive drugs.
When BP parameters were studied by ABPM in stages of CKD, it was observed that patients of stage IV were having uncontrolled SBP, DBP, MAP, and pulse pressure. The probable risk factors responsible for uncontrolled hypertension in these patients were irregular follow up and noncompliance to medication. Hence, it is important to optimize the BP control in these patients to decelerate the progression to stage V CKD.
In all stages of patients with CKD, the mean CBP measurements were significantly higher than mean ABPM measurements. Many of patients were labeled as uncontrolled HTN in spite of having controlled blood pressure by ABPM criteria. Hence, ABPM study helps in avoiding unnecessary change in medication in patients of CKD and harmful effects of hypotension. It is further important in our country as it decreases the financial burden on patients with respect to treatment cost.
We compared daytime and nighttime HBI in patients with CKD. In our study it was observed that the nighttime Systolic and diastolic HBI was significantly higher than daytime HBI with P < 0.001. The above results suggest that addition of the evening dose of antihypertensive drugs may help to achieve target BP at nighttime. The daytime and nighttime Systolic HBI in patients not on hemodialysis was higher than patients who were on hemodialysis. These results suggest that regular hemodialysis may help in decreasing the Hyperbaric Index in patients with CKD. These findings are giving insight into the need of adherence to drug treatment and regular dialysis in patients with CKD. In our study, the nighttime percentage time elevation was significantly higher than Daytime PTE, which can lead to more end-organ damage in patients with CKD.
The prevalence of systolic, diastolic, and MAP non-dippers was significantly higher in patients with CKD in our study. Similar results were observed in study by Farmer CK et al. 1997[15] and AASK[16] study where prevalence of non-dippers was 82% and 80% respectively. The significantly higher number of non-dippers reflects noncompliance to medications, inadequate medications and failure to administer evening time antihypertensive drugs. These could be the probable reasons for non-dipping phenomenon in these patients. In our study, we found that 83.33% patients of stage IV were systolic non-dipper and 84.4% patients of stage V CKD were systolic non-dippers. The above result suggested that prevalence of non-dipper was more in stage V patients with CKD than stage IV, so nocturnal BP control in these patients may help to decrease the progression of renal disease.
The prevalence of resistant hypertension in hypertensive patients with CKD was 39.66% (67 out of 169 patients). Similar results were found in cross-sectional cohort study of De Beus E et al., where the prevalence of resistant hypertension in male patients was 69%.[17] HBI and PTE[9] were significantly higher at nighttime than daytime in resistant HTN patients. In our study we found that total 38 patients out of 192 patients were having Early Morning Surge (19.79%), out of which 3 patients were in stage IV and 35 patients were in stage V. A study by Mizuno N in 2012,[18] suggested that the morning rise of BP in CKD patient is sustained type, that is, nocturnal blood pressure is elevated but not meeting the criteria for surge.
The study has limitations that it does not include stage I and II patients as the cohort under this study required indoor hospital admission.
Conclusion
Apart from mean pulse, mean systolic and diastolic BP and MAP, ABPM gives insight into various parameters of blood pressure which are useful in assessing the 24 h blood pressure control and target organ damage. ABPM being a noninvasive tool should be recommended in patients with CKD for detecting non-dipping phenomenon and impact on the target organs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors acknowledge the inputs by Mr. Kumar Naidu for statistical analysis of this study. Authors also acknowledge for Eris Life Sciences for their unconditional support in providing ABPM machine.
References
- What do we know about chronic kidney disease in India: First report of the Indian CKD registry? BMC Nephrol. 2012;13:10.
- [Google Scholar]
- A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: One-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR mHealth and uHealth. 2014;2:e57.
- [Google Scholar]
- 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127-248.
- [Google Scholar]
- Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793-801.
- [Google Scholar]
- Circadian systolic and diastolic hyperbaric indices of high school and college students. Chronobiologia. 1984;11:299-309.
- [Google Scholar]
- Hyperbaric area index calculated from ABPM elucidates the condition of CKD patients: The CKD-JAC study. Clin Exp Nephrol. 2015;19:114-24.
- [Google Scholar]
- Treatment of hypertension: Favourable effect of the twice-daily compared to the once-daily (evening) administration of perindopril and losartan. Kidney Blood Press Res. 2015;40:374-8.
- [Google Scholar]
- Factors influencing the development of end-stage renal disease. Clin Exp Nephrol. 2005;9:5-14.
- [Google Scholar]
- Chronic renal insufficiency cohort (CRIC) study: Baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4:1302-11.
- [Google Scholar]
- Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170-7.
- [Google Scholar]
- Sex disparities in control and treatment of modifiable cardiovascular disease risk factors among patients with diabetes: Translating research into action for diabetes (TRIAD) study. Diabetes Care. 2008;31:69-74.
- [Google Scholar]
- Blood pressure predicts risk of developing end-stage renal disease in men and women. Hypertension. 2003;41:1341-5.
- [Google Scholar]
- An investigation of the effect of advancing uraemia, renal replacement therapy and renal transplantation on blood pressure diurnal variability. Nephrol Dial Transplant. 1997;12:2301-7.
- [Google Scholar]
- The African American Study of Kidney Disease and Hypertension (AASK) trial: What more have we learned? J Clin Hypertens (Greenwich). 2003;5:159-67.
- [Google Scholar]
- Prevalence and clinical characteristics of apparent therapy-resistant hypertension in patients with cardiovascular disease: A cross-sectional cohort study in secondary care. BMJ Open. 2017;7:e016692.
- [Google Scholar]
- Morning hypertension in chronic kidney disease is sustained type, but not surge type. Blood Press Monit. 2012;17:20-3.
- [Google Scholar]







