Translate this page into:
Does Laparoscopic Omentectomy Reduce CAPD Catheter Malfunction: A Three-arm Pilot Randomized Trial
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Catheter malfunction secondary to omental wrapping is a frequent complication of continuous ambulatory peritoneal dialysis (CAPD). Of the various methods of peritoneal dialysis catheter insertion (PDCI), open surgical insertion under local anesthesia is most widely practiced. Laparoscopic omentectomy is often undertaken as a salvage procedure in case of malfunctioning catheters. However, there is no randomized controlled trial (RCT) to evaluate the role of prophylactic laparoscopic omentectomy on catheter function. This pilot RCT was undertaken to evaluate the impact of laparoscopic omentectomy on the incidence of catheter malfunction.
Materials and Methods:
Consecutive patients were randomized into three groups: laparoscopic PDCI with omentectomy (Group A), laparoscopic PDCI without omentectomy (Group B) and open surgical PDCI (Group C). The primary outcome was the incidence of catheter malfunction at 6 weeks and 3 months.
Results:
Forty-one patients completed follow-up, with 16, 11, and 14 patients in Groups A, B, and C, respectively. Incidence of catheter malfunction was 6.2%, 27.3%, and 14.3% in Groups A, B, and C, respectively, at 6 weeks and 6.2%, 36.4%, and 21.4% at 3 months, respectively. In patients with previously failed catheter insertion (n = 23), malfunction at 3 months was 8.3% (1/12) in patients who had omentectomy, compared with 45.5% (5/11) in those who did not (P = 0.069). Operating time was significantly higher (P < 0.001) in Group A.
Conclusions:
Laparoscopic omentectomy may be associated with a lower incidence of catheter malfunction, especially in patients with previously failed peritoneal dialysis catheter. Data from this pilot RCT can be used to design a large trial with an adequate number of patients.
Keywords
Chronic kidney disease
CKD
end-stage renal disease
peritoneal dialysis
renal replacement therapy Trial registration number: CTRI/2018/02/011871
Introduction
Continuous ambulatory peritoneal dialysis (CAPD) is an effective method of renal replacement therapy that helps preserve residual renal function in patients with end-stage renal disease (ESRD).[1] A properly positioned and patent dialysis catheter is paramount to successful CAPD. Various methods of insertion of CAPD catheter are in practice, namely, percutaneous, peritoneoscopic, laparoscopic, and open techniques.[2] Open surgical insertion under local anesthesia is the most commonly performed procedure. However, the open technique has certain disadvantages as it involves blind placement of the catheter, which may pose difficulty, especially in patients with obesity, previous laparotomy, or peritoneal adhesions. In comparison, laparoscopic technique allows accurate siting of the catheter in the pelvis under direct vision, and thus, may have less risk of catheter migration. However, laparoscopy requires general anesthesia, which carries its own risk, especially in patients with ESRD. Randomized studies comparing laparoscopic and open peritoneal dialysis (PD) catheter insertion (PDCI) have not shown any advantage of the former in terms of catheter survival.[34] A possible explanation could be that even with the laparoscopic technique, catheter malfunction is a frequent complication because of omental wrapping.
Prevention of omental wrapping by performing prophylactic omentectomy has been hypothesized and attempted in some centers.[56] However, performing omentectomy by open technique entails need for a long incision and can become a morbid surgery in patients with ESRD. Laparoscopic omentectomy is feasible and safe in experienced hands. Laparoscopy not only allows precise positioning of catheter under direct vision but also makes omentectomy easy and less morbid. This pilot randomized controlled trial (RCT) was undertaken to evaluate whether laparoscopic PDCI with or without omentectomy reduces the incidence of PD catheter malfunction.
Materials and Methods
This three-armed, parallel, pilot RCT was conducted at a tertiary referral center in northern India, after obtaining due clearance from the Institute Ethics Committee. The study was conducted jointly by the general surgery and nephrology departments. Informed written consent was taken from all patients.
Patient population
Consecutive patients, aged 1 to 80 years, referred from the Department of Nephrology for PDCI were considered for inclusion in the study. Patients who had previously undergone omentectomy or had contraindication for laparoscopic surgery (unable to withstand general anesthesia, uncontrolled bleeding disorder), pregnancy, ascites, active intraabdominal or parietal infection, gastrointestinal or urinary stoma, ventral or incisional hernia, or were unwilling to participate in the study were excluded. The principal investigator (AB) enrolled all patients in the study.
Randomization
Simple randomization was done using computer-generated random numbers in 1:1:1 allocation ratio by an independent statistician. Sequentially numbered, sealed, opaque envelopes were used to ensure concealed allocation. No blinding techniques were applied. The patients were randomized into three groups:
Group A – Laparoscopic PDCI with omentectomy under general anesthesia
Group B – Laparoscopic PDCI without omentectomy under general anesthesia
Group C – Conventional open surgical PDCI under local anesthesia
Demographic profile and clinical and laboratory data of all patients were collected and entered in a pre-structured proforma. Once the patients were in the operating room, the nursing in-charge was asked to open the sealed envelopes, and the patients were randomized to one of the three groups. Before surgery, the entry and exit sites of the catheter were marked by the surgeon. A dose of intravenous cefoperazone 1 g was given as surgical prophylaxis to all patients.
Laparoscopic technique
Laparoscopic PD catheter insertion was done by three senior consultants, each with at least 10 years of experience in laparoscopic surgery. After induction of general anesthesia in supine position with both hands by the side of the patient, pneumoperitoneum was created using a Veress needle inserted supra-umblically. A camera port and two working ports were placed in the left flank along the anterior axillary line. In case adhesions were encountered, adhesiolysis was done using blunt and sharp dissection. In the omentectomy group, the entire infracolic greater omentum was excised keeping the gastroepiploic arcade intact using ultrasonic cutting and coagulation device ensuring hemostasis. The omentum was then placed in an endobag and removed piecemeal through one of the working ports. Subsequent steps were similar in both Groups A and B. A 5-mm port was inserted above the umbilicus in midline through which a double-cuffed, 18 G straight Tenckhoff PD catheter was inserted and its tip positioned in the pelvis under vision. The catheter was exteriorized through a separate exit site (E) making a subcutaneous tunnel, 3 to 4 cm from the entry site. After desufflation of gas, inflow/outflow was tested with 500 mL heparinized saline. Fascial closure of ports was done with 1-0 polyglactin, and skin was closed with 3-0 nylon. No sutures were applied at the exit site.
Open technique
All open procedures were done by a single consultant with previous experience of more than 100 catheter insertions by open technique. The patient was placed supine, and the procedure was carried out under local anesthesia with 0.25% bupivacaine. A 3- to 4-cm infraumbilical midline incision was made and deepened up to the linea alba, which was incised, and the parietal peritoneum picked up with hemostats. A small nick was made in the peritoneum, and a finger was swept along the parietal peritoneum to break any adhesions. A double-cuffed, 18 G straight Tenckhoff PD catheter was introduced and directed towards the pelvis. The other end of the catheter was exteriorized through a subcutaneous tunnel. After confirming inflow and outflow, the cuff of the catheter was sutured to the peritoneum. Linea alba was closed with 2-0 polyglactin and skin with 3-0 nylon.
Operative data were recorded immediately after the operation. Data regarding operative time, postoperative recovery, and complications such as peritonitis, wound infection, catheter malfunction, pericatheter leakage, repositioning or change of catheter, and hospital stay were collected. Postoperatively, all patients had an X-ray imaging of abdomen to confirm the position of the catheter. PD was started 2 weeks after PDCI. The catheter was irrigated with 1 L of heparinized saline or dialysis solution after 72 hours of insertion and once weekly thereafter till the beginning of dialysis, to prevent blockage of catheter with fibrin plug. Follow-up was done in clinic at 1 week, 2 weeks, 4 weeks, 6 weeks, and 3 months. At each visit, functioning of the catheter and complications, if any, were recorded. Any additional procedure or admission after the index intervention was also recorded. Patients with malfunctioning catheters underwent X-ray imaging of abdomen after contrast injection through the catheter to check for obstruction or catheter tip migration. All data were entered in a prestructured pro forma.
Outcome measures
The primary outcome of the study was the incidence of catheter malfunction at 6 weeks and 3 months. Malfunction was defined as the presence of inflow or outflow restriction. Inflow restriction was defined as the inability of dialysis solution to flow freely into the peritoneal cavity. Outflow restriction was defined as outflow time longer than 30 minutes or retention of >30% of dialysate fluid. Malfunction was recorded by one of the investigators (AB), in the presence of the ward nurse in charge, at 6 weeks and at 3 months following the procedure. Operating time and complications were secondary outcomes.
Sample size
A sample size of convenience of 45 patients overall was chosen for this pilot trial.
Statistical analysis
Data were analyzed using Stata Version 14 (StataCorp, Texas) and presented in frequency and mean (standard deviation) or median (range). Both intention to treat (ITT) and per-protocol analyses were done. Analysis of variance followed by Bonferroni tests were applied to compare continuous data and Chi-square test or Fisher's exact test for categorical variables. A P value less than 0.05 was considered significant.
Results
Between September 2017 and September 2019, 59 consecutive patients, eligible for CAPD, were assessed. Fourteen patients were excluded for various reasons, and the remaining 45 were randomly allocated to Group A (n = 18), Group B (n = 12), and Group C (n = 15). Two patients in Group A discontinued PD, one in Group B was lost to follow-up, and one patient in Group C died 3 weeks after catheter insertion. In ITT analysis, these four patients were considered to have had catheter malfunction at both 6 weeks and 3 months. Per-protocol analysis was done excluding these four patients, with 16, 11, and 14 patients in Groups A, B, and C, respectively [Figure 1].
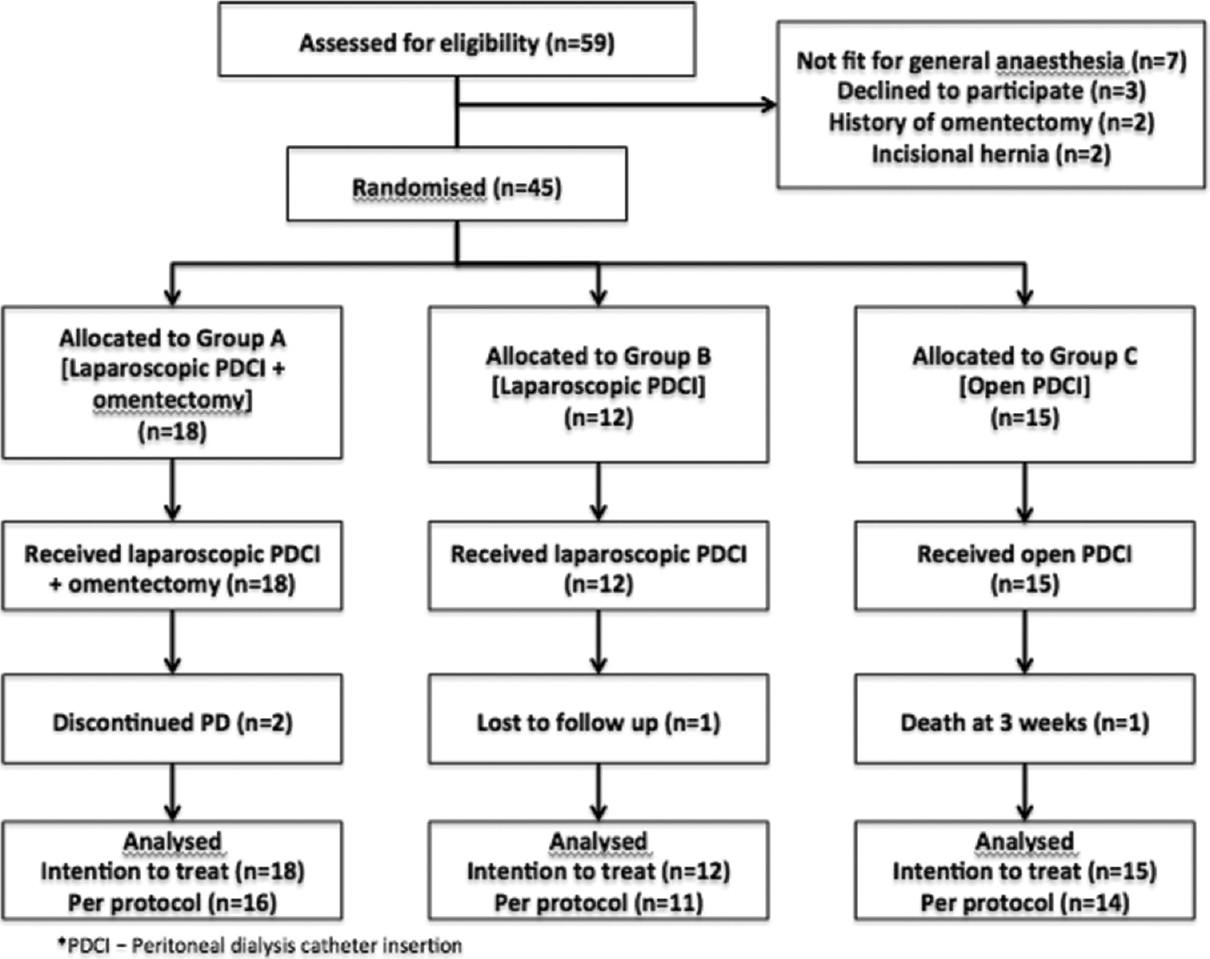
- CONSORT (Consolidated Standards of Reporting Trials) diagram
Baseline demographic and clinical characteristics of the study population are shown in Table 1. The mean age of the patients was 50.5 ± 21.3 years (range 4–82) and mean body mass index (BMI) was 23.2 ± 5.3 kg/m2 (range 13.9–34.6). The percentage of male patients was higher in Group C, but the difference was not significant. The known duration of chronic kidney disease was significantly higher in Group B (P = 0.02).
| Group A (n=18) | Group B (n=12) | Group C (n=15) | P | |
|---|---|---|---|---|
| Age, years (mean+SD) | 46±20.1 | 49.6±22.5 | 56.5±21.7 | 0.37 |
| Sex (Female:Male) | 6:12 | 5:7 | 2:13 | 0.26 |
| BMI, kg/m2 (mean+SD) | 24±6.4 | 23.1±4.9 | 22.4±4.1 | 0.68 |
| Duration of CKD, months (Range) | 1-180 | 5–168 | 4–98 | 0.02 |
| Duration of dialysis, months (Range) | 1-74 | 1-96 | 1-96 | 0.44 |
| Diabetes, n (%) | 9 (50) | 4 (33.3) | 9 (60) | 0.42 |
| Hypertension, n (%) | 18 (100) | 11 (91.7) | 14 (93.3) | 0.51 |
| CAD, n (%) | 4 (22.2) | 4 (33.3) | 6 (40) | 0.61 |
| Previous hemodialysis, n (%) | 17 (94.4) | 11 (91.7) | 10 (66.7) | 0.06 |
| Previous PD, n (%) | 12 (66.7) | 6 (50) | 6 (40) | 0.33 |
| Catheter malfunction | 11 | 3 | 5 | |
| PD peritonitis | 1 | 3 | 1 |
BMI=body mass index, CAD=coronary artery disease, CKD=chronic kidney disease, Group A=Laparoscopic peritoneal dialysis catheter insertion (PDCI) with omentectomy, Group B=Laparoscopic PDCI without omentectomy, Group C=Open PDCI, PD=peritoneal dialysis, SD=standard deviation
Primary outcome
Results of ITT and per-protocol analysis of the primary outcome are shown in Table 2. A functioning PD catheter was present in more than 85% patients (35/41) who followed up at 6 weeks. The incidence of catheter malfunction was 6.2% (1/16) in Group A, 27.3% (3/11) in Group B, and 14.3% (2/14) in Group C. Although the incidence of catheter malfunction was lower in Group A, the difference was not statistically significant.
| Intention to Treat Analysis (N=45) | ||||
|---|---|---|---|---|
| Group A (n=18) | Group B (n=12) | Group C (n=15) | P | |
| Catheter malfunction at 6 weeks, n (%) | 3 (16.7) | 4 (33.3) | 3 (20) | 0.598 |
| Catheter malfunction at 3 months, n (%) | 3 (16.7) | 5 (41.7) | 4 (26.7) | 0.306 |
| Per-Protocol Analysis (N=41) | ||||
| Group A (n=16) | Group B (n=11) | Group C (n=14) | P | |
| Catheter malfunction at 6 weeks, n (%) | 1 (6.2) | 3 (27.3) | 2 (14.3) | 0.344 |
| Catheter malfunction at 3 months, n (%) | 1 (6.2) | 4 (36.4) | 3 (21.4) | 0.169 |
| Mean catheter survival in months (range) | 11.8 (1-28) | 8.8 (0-20) | 9 (0-26) | 0.576 |
| Subgroup Analysis: First-Time PDCI (N=18) | ||||
| Group A (n=4) | Group B (n=6) | Group C (n=8) | P | |
| Catheter malfunction at 6 weeks, n (%) | 0 (0) | 1 (16.7) | 0 (0) | 0.556 |
| Catheter malfunction at 3 months, n (%) | 0 (0) | 2 (33.3) | 0 (0) | 0.137 |
| Subgroup Analysis: Previous Failed PDCI (N=23) | ||||
| Group A (n=12) | Group B (n=5) | Group C (n=6) | P | |
| Catheter malfunction at 6 weeks, n (%) | 1 (8.3) | 2 (40) | 2 (33.3) | 0.214 |
| Catheter malfunction at 3 months, n (%) | 1 (8.3) | 2 (40) | 3 (50) | 0.104 |
Group A=Laparoscopic PDCI with omentectomy, Group B=Laparoscopic PDCI without omentectomy, Group C=Open PDCI, PDCI=Peritoneal dialysis catheter insertion
At the end of 3 months, more than 80% catheters (33/41) were functioning. Between 6 weeks and 3 months, none of the patients in Group A had catheter malfunction; thus, the incidence of malfunction continued to be 6.2% in Group A. However, one more patient in Group B and one in Group C had catheter malfunction between 6 weeks and 3 months, increasing the incidence of malfunction to 36.4% and 21.4%, respectively. However, the difference continued to be statistically insignificant.
The patients were followed up till the time of writing this article. Mean catheter survival was 11.8 months (range 1–28), 8.8 months (range 0–20), and 9 months (range 0–26) in Groups A, B, and C, respectively (P = 0.576). The hazard ratios for catheter malfunction in Group B and Group C were 0.48 (95% CI 0.11–2.01) and 1.16 (95% CI 0.3–4.48), respectively.
Out of 41 patients, 18 were enrolled for PD treatment for the first time, whereas 23 had previously undergone at least one attempt at PDCI (i.e., failed insertion or malfunctioning catheter in situ or catheter removed due to complication). Among the 18 patients who underwent PDCI for the first time, one patient in Group B had catheter malfunction at 6 weeks and one at 3 months. None of the Group A or C patients in this subset had catheter malfunction till 3 months. However, more than half of the patients (23/41) in the study population were referred after failed PDCI done elsewhere. In this subgroup, the incidence of catheter malfunction at 6 weeks in Groups A, B, and C were 8.3%, 40%, and 33.3%, respectively. At 3 months, the incidence of catheter malfunction after open surgical insertion reached 50%; however, the difference was not significant. Results of these subgroup analyses are also shown in Table 2. In eight of these 23 patients, the previous catheter, which was in situ, could be salvaged by laparoscopic repositioning or freeing from omental wrap. Six of these eight patients had concomitant omentectomy.
Table 3 shows the impact of omentectomy on catheter patency. Patients with omentectomy had a lower malfunction rate (6.2%) at 6 weeks compared with those who did not have omentectomy (20%). At 3 months, the catheter malfunction rate further increased to 28% in patients who did not have omentectomy, compared with 6.2% in those who had omentectomy. However, the difference was not statistically significant.
| Whole Study Population (n=41) | |||
|---|---|---|---|
| Outcome | Omentectomy (n=16) | No omentectomy (n=25) | P |
| Malfunction 6 weeks, n (%) | 1 (6.2) | 5 (20) | 0.376 |
| Malfunction 3 months, n (%) | 1 (6.2) | 7 (28) | 0.12 |
| Subgroup: First-Time PDCI (n=18) | |||
| Outcome | Omentectomy (n=4) | No omentectomy (n=14) | P |
| Malfunction 6 weeks, n (%) | 0 (0) | 1 (7.1) | 0.999 |
| Malfunction 3 months, n (%) | 0 (0) | 2 (14.3) | 0.999 |
| Subgroup: Previous Failed PDCI (n=23) | |||
| Omentectomy (n=12) | No omentectomy (n=11) | P | |
| Malfunction 6 weeks, n (%) | 1 (8.3) | 4 (36.4) | 0.155 |
| Malfunction 3 months, n (%) | 1 (8.3) | 5 (45.5) | 0.069 |
PDCI: Peritoneal dialysis catheter insertion
In the subgroup of previously failed PDCI, the incidence of catheter malfunction at 6 weeks was 8.3% in patients who had omentectomy, compared with 36.4% in those who did not. At 3 months, there was a trend toward statistical significance (P = 0.069) with a catheter malfunction rate of 45.5% in patients who had not undergone omentectomy [Table 3].
Secondary outcomes
Operating time was significantly higher (P < 0.001) in Group A (60 minutes) compared with Group B (34 minutes) and Group C (26 minutes). The three groups were comparable in terms of intraoperative and postoperative morbidity [Table 4]. One patient in Group C had intraoperative bleeding. The patient was on aspirin, which was withheld in the postoperative period. He developed operative site hematoma in the postoperative period, which was managed conservatively. Transfusion of blood products was not required. In another patient in Group C, the PD catheter could not be introduced even after repeated attempts due to intraperitoneal adhesions. The incision was sutured, and catheter insertion was done through a separate incision. One patient each in Groups A and B had PD peritonitis at 6 weeks; both were managed with intraperitoneal antibiotics and did not require catheter removal. One patient in Group A had a surgical site infection in the postoperative period, which was managed by the opening of skin sutures, daily dressing, and intravenous antibiotics. One patient in Group A developed hypoxia on extubation and had to be reintubated on table. He was subsequently extubated on postoperative Day 1 and had an uneventful recovery thereafter. One patient in Group C had a sudden death at 3 weeks; at that time, his catheter was fully functional.
| Group A (n=16) | Group B (n=11) | Group C (n=14) | P | |
|---|---|---|---|---|
| Operating time (min) Mean±SD | 59.7±33 | 34.2±14.1 | 25.9±9.6 | <0.001 |
| Overall complications, n (%) | 3 | 1 | 2 | 0.87 |
| Bleeding, n (%) | 0 | 0 | 1 | 0.6 |
| Other intraoperative complications, n (%) | 1 | 0 | 1 | 0.999 |
| PD peritonitis, n (%) | 1 | 1 | 0 | 0.704 |
| SSI, n (%) | 1 | 0 | 0 | 0.999 |
Group A=Laparoscopic PD catheter insertion with omentectomy, Group B=Laparoscopic PD catheter insertion without omentectomy, Group C=Open PD catheter insertion, PD=peritoneal dialysis, SD=Standard deviation, SSI=surgical site infection
Discussion
This pilot trial is the first randomized study attempting to evaluate the role of laparoscopic omentectomy on PD catheter function. Follow-up at 3 months was more than 90%, and all the patients underwent the treatment that was allocated; there was no crossover. Only one out of 16 patients undergoing omentectomy had catheter malfunction, which, on re-laparoscopy, was found to be due to small bowel adhesions. Although the difference in catheter malfunction among patients with and without omentectomy did not reach statistical significance, the reduction in malfunction in the former was clinically relevant.
One of the most frequent complications of PD is catheter malfunction due to mechanical obstruction secondary to omental wrapping, kinking, or migration of the catheter. Proponents of laparoscopy claim that catheter insertion under vision results in a higher success rate due to accurate placement of the tip of the catheter in the pelvis. However, two meta-analyses comparing laparoscopic and open PDCI reported contradictory results. Xie et al.,[7] in a meta-analysis of four randomized trials and 10 observational studies, found longer operating time in laparoscopic PDCI and no difference in hospital stay, early and late complications, including catheter migration and blockage. In another meta-analysis of three randomized trials and eight cohort studies, Hagen et al.[8] found a lesser incidence of catheter migration and greater 1-year catheter survival in the laparoscopic approach. In a recent multicenter randomized trial comparing laparoscopic and open PDCI (CAPD I trial), van Laanen et al.[3] compared catheter function 2 to 4 weeks after insertion. Adequate function was seen in 77% of patients having open insertion and 70% of patients having laparoscopic insertion. The difference was statistically not significant, and morbidity in the two groups was comparable. The authors commented that laparoscopy-assisted catheter fixation and omentectomy might improve catheter survival. The CAPD II trial is currently underway to study this objective. In another randomized trial from the United Kingdom, Wright et al.[4] found conventional surgery to be significantly faster than laparoscopic surgery. Catheter survival and early and late complications were comparable. Our results were similar, with the incidence of catheter malfunction at 3 months being 36.4% and 21.4%, respectively, for laparoscopic (without omentectomy) and open techniques. In a randomized trial of first-time PDCI from Taiwan, 77 patients were randomly allocated to open or laparoscopic insertion. Catheter longevity was comparable in the two arms. The authors recommended conventional open insertion for patients having primary catheter placement, as it was more cost-effective.[9] Similarly, in patients undergoing PDCI for the first time, we did not find any advantage of a laparoscopic approach. However, when performing omentectomy, laparoscopy is the preferred approach as it allows removal of the omentum through 1- to 2-cm incisions, which otherwise would require a long incision, resulting in increased morbidity.
Several authors have proposed partial omentectomy to reduce the incidence of catheter malfunction due to omental wrapping. Omentum has a natural tendency to wrap around any foreign body in the peritoneal cavity and isolate it from the rest of the abdomen. Omental wrapping around the catheter causes occlusion of the side holes or tip of the catheter, which is clinically manifested as outflow obstruction.[10] Reissman et al.[5] performed routine omentectomy in 60 consecutive patients under local anesthesia. There was only one (2%) catheter obstruction during a mean follow-up of 28 months and 90% of the catheters survived 1 year. Nicholson et al.[6] performed omentectomy in 113 cases out of 300 consecutive open PD catheter insertions. Catheter survival was significantly higher in the patients having omentectomy (78%, compared with 50% without omentectomy, P = 0.0002). In a retrospective study by Kavalakkat et al.,[11] 40 patients underwent omentectomy and PDCI, whereas 18 underwent PDCI only. None of the patients undergoing omentectomy developed catheter blockage, whereas 27.8% of patients in the other group did. In a study by Sanderson et al.,[12] routine omentectomy in 260 patients undergoing CAPD catheter placement resulted in 60% reduction in catheter obstruction. One-year catheter survival was 90%. In our study, omentectomy resulted in a malfunction rate of 6.2% at 3 months, compared with 28% without omentectomy. Our results, though statistically not significant, are in concordance with these studies.
Although prophylactic omentectomy during open PDCI has shown promising results in terms of catheter survival, there is no large series of laparoscopic prophylactic omentectomy. Laparoscopic insertion and omentectomy are more often recommended as a salvage procedure for blocked PD catheters.[10131415] A purported advantage of laparoscopic PDCI (in addition to facilitating omentectomy through small incisions) is that it also facilitates lysis of intraperitoneal adhesions. Patients who have had previous abdominal surgery or PD peritonitis are more prone to adhesion formation. In the open technique of PDCI, it is difficult to lyse these adhesions without resorting to a long incision, with its attendant morbidity. Patients with previous failed PD catheter comprised a major fraction (53%, n = 24/45) of our study population. These patients either had removal of their previous catheter due to intractable or fungal peritonitis, or came with a catheter in situ, with outflow failure. Laparoscopic insertion and/or omentectomy in such situations may be advantageous. Yilmazlar et al.[14] reported 16 cases of malfunctioning catheter, of which 13 were salvaged using adhesiolysis (n = 8) or catheter repositioning (n = 5). Peppelenbosch et al.[15] successfully managed 18 out of 23 patients with catheter malfunction using a combination of advanced laparoscopic techniques, including catheter repositioning (n = 23), fixation (n = 21), omentectomy (n = 8), and adhesiolysis (n = 3). Lee and Donovan[13] performed omentectomy in 13 patients with catheter malfunction; five patients had recurrent catheter malfunction, of which three were managed with laparoscopic manipulation. In our study, the previous catheter was salvaged in eight patients, of which six underwent omentectomy and two had simple laparoscopic repositioning without omentectomy. In patients with previous failed PDCI, omentectomy led to a fivefold reduction (8.3% vs. 45.5% in no omentectomy) in malfunction at 3 months. Thus, laparoscopic omentectomy seems to be beneficial in this subset of patients.
Important disadvantages of the laparoscopic technique are the need for general anesthesia with its attendant risks, prolonged operating time, and the need for expensive laparoscopic setup and instruments. In a recent Indian study, in which 19 patients with malfunctioning catheters underwent laparoscopic salvage procedure with omentopexy, the median operating time was 63 minutes, and there were no intraoperative or postoperative complications.[16] In the study by Kavalakkat et al.,[11] operating time was significantly higher in patients who had omentectomy (90 minutes vs. 80 minutes in patients without omentectomy). Similar results were observed in our study; on an average, omentectomy took about 26 minutes more. However, the low rate of intraoperative complications (6.2%, n = 1/16) in our study confirms that laparoscopic PDCI with omentectomy is a safe procedure. In a recent multicenter collaborative cohort study from USA, the incidence of early PD peritonitis (defined as peritonitis within 60 days of insertion of a catheter) was 8.4%.[17] The incidence of early PD peritonitis (within 3 months) in our study was also relatively low (4.9%) and comparable among the three groups. This is in contrast to a recent Turkish study, in which the authors found a significant higher rate of peritonitis in open insertion (75%) compared with laparoscopic insertion (25%). The high rate of peritonitis in this study is not surprising, as this was a 12-year-long study with longer follow-up.[18]
Our study is limited by inadequate sample size and short follow-up. Block randomization was not done, leading to unequal distribution of patients in the three groups. The high proportion of patients with prior failed PD catheter is also a shortcoming, as these patients may be more likely to benefit from laparoscopic omentectomy. Despite these limitations, the results of our study may be clinically relevant. We chose to conduct a pilot trial as the majority of ESRD patients in our setup are reluctant to opt for PD and prefer hemodialysis as renal replacement therapy. PD. Future research should also be focused on cost–benefit analysis of surgical PD catheter insertion techniques in the Indian setting.
In conclusion, this study found a statistically nonsignificant but clinically relevant reduction of catheter malfunction in patients undergoing laparoscopic omentectomy, especially in those with previous failed PD catheters. High-quality trials with adequate number of patients are required before this can be routinely practiced.
Ethics approval
The study was approved by the Institute Ethics Committee (Ref. no. IECPG-398/07.09.2017) and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed written consent was obtained from all participants included in the study.
Acknowledgments
The authors would like to thank Mr. Ashish Dutt Upadhyay (Department of Biostatistics), Dr. Akhil Goel (Associate Professor, Department of Community and Family Medicine, All India Institute of Medical Sciences, Jodhpur), and the residents of the Department of Nephrology, All India Institute of Medical Sciences, New Delhi, for their contribution.
Financial support and sponsorship
The first author has received financial support from the Indian Council of Medical Research (ICMR) for this study. The ICMR was not involved in study designing, collection, analysis, or interpretation of data, or in the decision to submit the article for publication.
Conflicts of interest
There are no conflicts of interest.
References
- Peritoneal dialysis and preservation of residual renal function. Perit Dial Int. 2009;29((Suppl 2)):S108-10.
- [Google Scholar]
- Percutaneous peritoneal dialysis catheter insertion by a nephrologist: A new, simple, and safe technique. Perit Dial Int. 2014;34:204-11.
- [Google Scholar]
- Randomized controlled trial comparing open versus laparoscopic placement of a peritoneal dialysis catheter and outcomes: The CAPD I trial. Perit Dial Int J. 2018;38:104-12.
- [Google Scholar]
- Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int. 1999;19:372-5.
- [Google Scholar]
- Placement of a peritoneal dialysis catheter with routine omentectomy--Does it prevent obstruction of the catheter? Eur J Surg Acta Chir. 1998;164:703-7.
- [Google Scholar]
- The role of omentectomy in continuous ambulatory peritoneal dialysis. Perit Dial Int. 1991;11:330-2.
- [Google Scholar]
- Laparoscopic versus open catheter placement in peritoneal dialysis patients: A systematic review and meta-analysis. BMC Nephrol. 2012;13:69.
- [Google Scholar]
- Laparoscopic versus open peritoneal dialysis catheter insertion: A meta-analysis? PLoS One. 2013;8:e56351. doi: 10.1371/journal.pone.0056351
- [Google Scholar]
- Prospective randomized study for comparison of open surgery with laparoscopic-assisted placement of Tenckhoff peritoneal dialysis catheter--A single center experience and literature review. J Surg Res. 2010;159:489-96.
- [Google Scholar]
- Laparoscopic omentectomy for peritoneal dialysis catheter flow obstruction: A case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 1999;9:228-33.
- [Google Scholar]
- Continuous ambulatory peritoneal dialysis catheter placement: Is omentectomy necessary? In: Urol Ann. Vol 2. Mumbai, India: Medknow Publications Pvt. Ltd; 2010. p. :107-9.
- [Google Scholar]
- Surgical complications of continuous ambulatory peritoneal dialysis. Am J Surg. 1990;160:561-5.
- [Google Scholar]
- Laparoscopic omentectomy for salvage of peritoneal dialysis catheters. J Endourol. 2002;16:241-4.
- [Google Scholar]
- Laparoscopic management of malfunctioning peritoneal dialysis catheters. Surg Endosc. 2001;15:820-2.
- [Google Scholar]
- Revision techniques for failed PD catheters: Outcome in a University Hospital. J Vasc Access. 2015;16((Suppl 9)):S93-5.
- [Google Scholar]
- Minimally invasive surgery for salvage of malfunctioning peritoneal dialysis catheters. J Minim Access Surg. 2019;15:19-24.
- [Google Scholar]
- Risk factors for early onset peritonitis: The SCOPE collaborative. Pediatr Nephrol. 2019;34:1387-94.
- [Google Scholar]
- Single port laparoscopic and open surgical accesses of chronic peritoneal dialysis in children: A single center experience over 12 years. J Minim Access Surg. 2016;12:162-6.
- [Google Scholar]







